Tuberculosis
tuberculosis (abbreviated TB or TB), alternatively and historically called consumption (from the Greek φθίσις, via Latin phthisis), is a contagious bacterial infection that affects the lungs, but can spread to other organs. The most important and representative species of bacteria that causes tuberculosis is Mycobacterium tuberculosis or Koch's bacillus, belonging to the Mycobacterium tuberculosis complex. There is a vaccine (BCG) to prevent this disease.
It is perhaps the most prevalent infectious disease in the world. Considering its latent form, in which it does not present symptoms, it is estimated that it affects 33% of the world population. It is the second global cause of death, and the first among infectious diseases.
Other mycobacteria, such as Mycobacterium bovis, Mycobacterium africanum, Mycobacterium canetti, and Mycobacterium microti can cause tuberculosis, but all these species do not usually do so in a healthy individual.
The symptoms of tuberculosis are: chronic cough with bloody sputum, fever, night sweats and weight loss. Infection of other organs causes a wide variety of symptoms.
Diagnosis is based on radiology (chest x-rays), a tuberculin skin test and blood tests, as well as microbiological examination and microbiological culture of body fluids such as sputum. Treatment is complicated and requires long periods of exposure to antibiotics. The relatives of the patient are also analyzed.
In recent years, tuberculosis has shown increasing resistance to multiple antibiotics and for this reason, vaccination campaigns have been chosen as a preventive measure, generally with the Bacillus Calmette-Guérin (BCG) vaccine.[citation required]
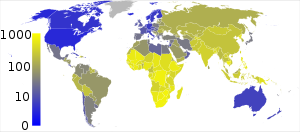
It is spread through the air when infected people cough, sneeze, or spit. In addition, a growing number of people around the world contract it because their immune systems are weakened by immunosuppressive drugs or AIDS. The distribution of tuberculosis is not uniform in the world; 80% of the population of Asian and African countries test positive, a percentage that drops to 5-10% of the population in the United States.
According to data from the World Health Organization (WHO), in 2013 nine million people fell ill with tuberculosis and 1.5 million died from this cause, of whom 360,000 had HIV infection. About 60% of cases and deaths occur in men. Of the 510,000 women who died from this cause in that period, more than a third had HIV infection. The WHO estimates that early diagnosis and effective treatment saved 37.2 million people between 2000 and 2013, but considers the number of these preventable deaths "still unacceptably high".
Signs and symptoms
Tuberculosis can be manifested by clinical signs and pulmonary or extrapulmonary symptoms.
Pulmonary tuberculosis
- Tuberculosis pneumonia: may be due to first-infection or reactivation, although primary infection usually causes few symptoms (paucithematic). First-infection is characterized by the formation of the primary complex of Ghon (parahyliar regional adenitis, lymphangitis and pneumonitis). The clinic in revival is usually insidious, with a fever and general discomfort. Night sweating and weight loss are common. As for pulmonary semiology, there are usually persistent coughs that may be accompanied by hemoptoic sputums (sanguinolent). Tuberculosis pneumonia is very contagious, its patients must be isolated for two weeks from the beginning of the treatment.
- Tuberculosis Pleuritis: It appears in young people and usually does so acutely and unilaterally. The main sign is an exudate in the pleural space. Characteristic of this exudate is that the elevated adenosin-desaminese enzyme (ADA) is detected. The predominant cell type in the exudate are lymphocytes and mesothelial cells are scarce.
Extrapulmonary Tuberculosis
Extrapulmonary tuberculosis can appear in the context of miliary tuberculosis, the reactivation of a pulmonary focus or in the absence of clinical pulmonary disease. Includes:
- Meninegeal Tuberculosis: Form of bacterial meningitis caused by Mycobacterium tuberculosis or more rarely Mycobacterium bovis. The organism settles in the meninges, predominant in the encephalic base, and microgranulomas form with subsequent breakage. The clinical course tends to be subbagudo, which progresses in days. Symptoms may be: headache, nuc stiffness, neurological deficits.
- Ocular Tuberculosis: tuberculosis infection of iris, ciliar bodies and choroids.
- Cardiovascular tuberculosis: TB that affects human heart, pericardial or blood vessels. Tuberculosis pericarditis can evolve to constrictive pericarditis, which leads to the use of corticosteroids in its treatment.
- Tuberculosis of the central nervous system: brain tuberculosis, spinal cord or meninges. Caused by Mycobacterium tuberculosis Or, weirder, by Mycobacterium bovis.
- Genitourinary tuberculosis: usual cause of sterile piuria (leucocytes in urine without visible germ). The access of the infection to the genitourinary system is usually by blood. It can be a cause of sterility due to the involvement of epidimos in men and fallopian tubes in women.
- Nodal tuberculosis: compromises cervical and supraclavicular nodal chains. It causes swelling of the lymph nodes. It can present scrofulodermy: swelling of the local extension of the subcutaneous tissue due to a reactivation of the tuberculous bacillus in those tissues. In this case, fistulas or draining ulcers are produced, presenting fibrosis and induration in addition to dark reddish. It is common in young people and children. In infants it is very common for the infection to occur in superficial nodes accompanied by fistulas. 50% of cases, both in young and in children, the disease is manifested with severe swelling of the cervical nodes. The swollen node is presented in physical exploration as a large painful mass with probable fistulation (scroful). Such fistulation (scrofulodermy) is usually dark red. In all cases there is a fever.
- Osteoarticular tuberculosis: After a lung infection, the sludge can circulate through the bloodstream to stay in some bone or joint, this would be a tuberculosis osteoarthritis or osteoarticular tuberculosis. Tuberculosis osteomyelitis may also appear without joint involvement, although its frequency is low. The infection may be caused by a wound caused by an object contaminated with the bacillus, although no one is documented in this way. In the 1930s, treatments were carried out with carbon arc light with disparate results.
- Disseminated (miliary tuberculosis)
- Miliar Tuberculosis: form of tuberculosis due to the blood dissemination of the bacillus, affecting different organs. It happens in people with severe immune system disruption. It's more common in the elderly. You can study with acute or insidious start. Symptomology is dominated by fever and other constitutional symptoms. For diagnosis, any or all of the following crops should be practiced: sputum, urine, gastric juice or bone marrow.
- Intestinal tuberculosis.
Transmission
Tuberculosis can only be transmitted by people with active disease. TB is transmitted through particles expelled by the smear-positive patient (with active TB) when coughing, sneezing, speaking, spitting, etc., so it is recommended not to have contact with third parties. Infectious droplets (flügge's or droplets) have a diameter between 0.5 to 5 µm, around 400,000 can be produced with a single sneeze. Each of these droplets from an active patient can transmit the microorganism, especially knowing that the infectious dose of tuberculosis is considered low, so that the inhalation of a single bacterium can infect. The probability of an effective transmission increases with the number of contaminated particles expelled by the patient, in how good it is the ventilation of the area, the duration of exposure and the virulence of the M. tuberculosis. People with frequent, prolonged, or intense contacts have a risk of around 25% of being infected. For a smoker, the chances of getting sick are multiplied by 2.5. A patient with active TB without treatment can infect between 10-15 people per year. Other risks include those areas where TB is prevalent, in immunocompromised patients with conditions such as malnutrition and AIDS, high-risk ethnic populations, and health care workers serving in high-risk regions. In AIDS patients, TB acts as a disease opportunistic (co-infection) with strong association. It can also be transmitted through the digestive tract, especially by ingesting unsanitized milk from tuberculosis cows infected with Mycobacterium bovis.
The chain of transmission can be broken by isolating the patient with active TB and immediately starting effective anti-TB therapy. After two weeks with such treatment, those patients with active and non-resistant TB are no longer contagious. If a person were to become infected, it will take less than 20 to 60 days before he can begin to spread the disease to others.
Clinical picture of tuberculosis
In the beginning of the disease, people with tuberculosis may have symptoms common to other diseases, such as fever, tiredness, lack of appetite, weight loss, depression, night sweats and dyspnea in advanced cases; more when the afflictions of cough and purulent expectoration are added for more than fifteen days it must be studied, since it is considered a respiratory symptom.
In about 25 percent of active cases, the infection spreads from the lungs, causing other forms of tuberculosis. This occurs more frequently in immunosuppressed patients and in children. Extrapulmonary infections include the pleura, the central nervous system causing meningitis, the lymphatic system causing scrofula of the neck, the genitourinary system causing urogenital tuberculosis, and the bones or joints in the case of Pott's disease. A very serious form of disseminated is miliary tuberculosis. Although extrapulmonary tuberculosis is not contagious, it can coexist with contagious pulmonary tuberculosis.
History
Tuberculosis is one of the oldest human diseases. Although estimated to be between 15,000 and 22,000 years old, it is more widely accepted that this species evolved from other more primitive microorganisms within the genus Mycobacterium. It may be thought that at one point, some species of microbacteria would cross the biological barrier, due to selective pressure, and would have a reservoir in animals. This may have given rise to an ancient progenitor of Mycobacterium bovis, accepted by many to be the oldest of the Mycobacterium tuberculosis complex species, which includes M. tuberculosis, M. bovis, M. africanum and M. microti. The "step" The next step would be the M. bovis to the human species, coincides with the domestication of animals. Thus it could have emerged as a pathogen for the dog.
Pathogenesis of tuberculosis
Tuberculosis is a paradigm of the interaction of an exogenous agent and the host's immune response. The World Health Organization estimates 2 billion infected by M. tuberculosis and eight million new infections every year, winning the battle in most cases. However, almost two million people a year die from this disease.
- Latent tuberculosis infection: infection M. tuberculosis usually performed by air. In this way, the bacillus is made by the alveolar macrophages. In 30% of cases, these macrophages are unable to destroy it. Then the infection is generated, which is characterized by growth within the phgosoma of infected macrophages. This is because the bacillus is able to stop the fago-lisosoma union. From histopathology, a granuloma is generated in the focus of infection, characterized by the presence of intragranulomatous necrotic tissue and which is finally structured with the acquisition of immunity. With immunity, infected macrophages can activate and destroy the sludge, so that its concentration is controlled.
Then the latent infection begins, characterized by the presence of a specific immune response, control of the bacillary concentration, but with the presence of latent bacilli (in steady state) in the necrotic tissue. As macrophages drain this tissue, dormant bacilli blend in with this necrosis and are drained into the alveolar space, where they can resume growth again. In this way the infection is maintained for years.
From a clinical point of view, latent tuberculosis infection does not cause symptoms. Its diagnosis is based on the Mantoux skin test. Individuals with this infection cannot infect anyone. However, in 10% of cases, control of the bacillary concentration is lost, growth resumes and active tuberculosis or tuberculosis itself can be generated. Therefore it should be treated, especially newly infected patients. The treatment represents the administration of isoniazid for 9 months, a fact that makes follow-up difficult.
Progression
Progresses from tuberculosis infection to tuberculosis disease. It can occur early (primary tuberculosis, around 1-5%) or several years after infection (postprimary tuberculosis, secondary, tuberculosis reactivation in around 5-9%). The risk of reactivation is increased with alterations in the immune system, such as those caused by HIV. In patients coinfected with HIV and TB, the risk of reactivation increases by 10% per year, while in an immunocompetent person the risk is 5-10% throughout life.
Some drugs, including treatments used in rheumatoid arthritis that block tumor necrosis factor, increase the risk of activation of latent TB due to the important action of this cytokine in the immune response against TB.
Diagnosis
Active TB is diagnosed by detecting Mycobacterium tuberculosis in any sample from the respiratory tract (pulmonary TB) or outside of it (extrapulmonary TB). Although some more modern methods (molecular diagnosis) have been developed, microscopic vision of acid-fast bacilli (AFB) and culture in Löwenstein-Jensen medium remain the gold standard for the diagnosis of TB, especially in countries with low health resources, although the MODS method has been validated, giving results with greater sensitivity and specificity than culture. AFB microscopy is fast and cheap and a very efficient method to detect contagious patients. Cultures are used in TB when there is a low bacterial load (greater sensitivity), to identify the strain and to study sensitivities to different treatments. Both microscopy and culture can be used to monitor treatment.
Autofluorescence
The Autonomous University of Madrid published a paper in the Journal of Clinical Microbiology where it is described for the first time that mycobacteria are capable of emitting fluorescence, which allows them to be seen under a fluorescence microscope without the need for from a previous staining. This characteristic is of interest for the diagnosis of tuberculosis, since it was previously necessary to resort to specific stains to be able to observe most of the bacteria, since very few present autofluorescence. However, the autofluorescence emitted by sky-blue mycobacteria is just as intense and bright as when stained green with the old method. In addition, it has been verified that the phenomenon is permanent, autofluorescence does not decrease with the passage of time, so special conservation of the samples is not necessary for its maintenance.
Chest X-ray
X-rays are essential in the diagnosis of the disease. The typical radiological lesions are apical, in the right hemithorax, in posterior segments and generally form cavities.
The diagnostic tool for tuberculosis cases is bacteriology (smear microscopy and culture) due to its high specificity, sensitivity, and predictive value. In those situations where the bacteriological studies are not conclusive, it will be necessary to carry out diagnostic follow-up in accordance with the organization of the health services network, using other criteria: clinical, epidemiological, imaging, immunological, pathological.
Anyone diagnosed with tuberculosis after counseling and acceptance must undergo a diagnostic test for HIV.
Sputum smear microscopy
It consists of a serial test (three consecutive days), where a sputum sample is taken to see what bacteria are found. With a low cost and rapid execution, smear microscopy is a technique that allows the identification of 70-80% of positive pulmonary cases. The bacterium Mycobacterium tuberculosis has a different wall structure from those that are capable of being typified by Gram staining, as they present a very abundant amount of lipids. It is called acid-alcohol resistant and this characteristic is what allows its observation by the Ziehl Neelsen stain.
Biological sample culture
The culture can be done in the Löwenstein-Jensen medium, which is made up of:
- egg (albumin, lipids) (coagula and gives solidity)
- Malachite green (inhibites other bacteria)
- glycerol (carbon source)
- asparagins (nitrogen source)
Grows very slowly (30 to 90 days) at 37 °C in an atmosphere with carbon dioxide (in culture they grow better despite being strictly aerobic), giving colonies with the appearance of breadcrumbs (or spider eggs), dry yellowish and rough.
Mantoux tuberculin skin test
It is a skin test (intradermal reaction) to detect tuberculosis infection. PPD (Purified Protein Derivative) is used as a reagent. The Mantoux tuberculin test only involves contact, not infection.
MODS (Microscopic observation drug susceptibility)
Mycobacterium tuberculosis drug susceptibility by microscopic observation (MODS) is a recently developed method that has very high sensitivity and specificity, as well as greatly reducing the time to diagnosis of Mycobacterium tuberculosis infection. , while also evaluating resistance to first-line antibiotics such as isoniazid and rifampicin for MDR-TB (multidrug-resistant) patients.
Treatment
The treatment of tuberculosis is carried out with combinations of anti-tuberculous drugs, making the guidelines of six months of treatment effective, two in the first phase of treatment and four months in the second phase.
TB is curable, but early diagnosis (see a doctor right away) is necessary, as it is a serious disease if treatment is not followed. In addition, it is essential not to abandon the treatment given by the doctor because, by suspending it, the disease worsens rapidly and favors the proliferation of drug-resistant bacilli.
Sanatorical treatment of tuberculosis
It began in the middle of the 19th century and the first half of the 20th, it became generalized as the basis of treatment, especially in developed countries, it became one of the indices that determine the health level of a country.
Sanatoriums were built at high altitudes, based on the physiological theory of increasing pulmonary blood flow, due to altitude-induced tachycardia. However, the evidence for its efficacy was dubious.
Surgical treatment of tuberculosis
Various techniques were performed, all of them based on collapse therapy, which consisted of making the lung collapse so that it would remain at rest and thus help heal the lesions.
- Procedures:
- First rib condrotomy
- Toracoplasties (amputing a number of ribs to get the collapse)
- Lung remedies
- Frenicectomy (female nerve section to paralyze diaphragm)
- Bathing ladder (section of the ladder muscles)
- Extrapleural Pneumolisis
- Therapeutic pneumothorax: Perhaps the most frequently performed surgical procedure
Pharmacological treatment of tuberculosis
The history of tuberculosis changes after the introduction of antibiotic agents. The treatment of tuberculosis is fundamental for its control, since with it the chain of transmission is broken when the treatment is correct and is followed completely.
Pharmacological treatment began in 1944 with streptomycin (SM) and para-aminosalicylic acid (PAS). In 1950, the first clinical trial was conducted comparing the efficacy of SM and PAS together or as monotherapy. The study showed that the combination therapy was more effective. In 1952, a third drug, isoniazid (INH), was added to the combination, dramatically improving the efficacy of treatment, although still lasting 18-24 months. Ethambutol was introduced in 1960, replacing PAS in treatment schemes and reducing the duration to 18 months. In the 1970s, with the introduction of rifampicin (RAM) in the combination, the treatment was shortened to nine months. In 1980, pyrazinamide (PZA) was introduced into the therapeutic regimen, which could reduce it to six months.
Two biological facts explain why combination therapy is more effective in treating TB than monotherapy. The first is that treatment with a single drug induces the selection of resistant bacilli and consequently the failure to eliminate the disease. The second is that different bacillary populations can coexist in one patient.
Antituberculostatics are classified into two groups based on their efficacy, potency, and side effects:
- Frontline drugs: isoniac, rifampicin, pirazinamide, etambutol or streptomycin
- Second-line drugs: cycline, etionamide, ciprofloxacin, etc. They are used in cases of resistant TB or when frontline TBs produce side effects.
A problem that has spread in recent years is the appearance of M. tuberculosis resistant to antibiotics. Taking into account the resistance to antibiotics that different strains present, it is possible to distinguish between multi-resistant strains (MDR), which are bacteria that develop resistance against rifampicin (RMP) and isoniazid (INH), and ultra-resistant strains (XDR), resistant to first-line drugs and to any member of the fluoroquinolone family, and at least one second-line drug.
Prevention
It is prevented through a healthy and hygienic life, with early identification of the sick and ensuring their cure so as not to infect other people, through the BCG vaccine.
Systematic BCG vaccination of newborns was abandoned in Spain in 1980.
Preventive measures
- The infected person must be protected whenever he coughs with disposable tissues.
- Hand wash after coughing.
- Appropriate ventilation of the residence.
- Clean the domicile with damp cloths.
- Use mask in common areas.
- Restrict visits to people not exposed to the disease.
- Guarantee adherence to treatment.
- No smoking. Cigarette does not cause tuberculosis, but it does favor the development of the disease.
Vaccines
BCG
The BCG (Bacillus Calmette-Guérin) vaccine, used since 1921, is still used in many countries as part of tuberculosis control programs, especially in children. This vaccine was developed at the Pasteur Institute, France, between 1905 and 1921. However, mass vaccinations did not begin until after World War II. The protective efficacy of BCG in severe forms of tuberculosis (p. g.: meningitis) in children under 4 years of age is great (BCG protects against M. tuberculosis infection as well as against progression from infection to disease. systematic review and meta-analysis was performed in vaccinated and unvaccinated children under 16 with recent exposure to tuberculosis infection), and is around 80%; its efficacy in adolescents and adults is more variable, being between 0 and 80%.
RUTI
RUTI is a therapeutic vaccine being developed at the Badalona Experimental Tuberculosis Unit (Spain) to reduce the treatment of latent tuberculosis infection from 9 to 1 month of isoniazid administration. Responsible are Archivel Farma and the Germans Trias i Pujol Hospital in Badalona, known as Can Ruti, which has given the vaccine its name.
MTBVAC Vaccine
MTBVAC is the first attenuated human tuberculosis bacillus vaccine. The current BCG is from bos taurus. The group from the University of Zaragoza, led by the researcher Carlos Martín Montañés, in collaboration with the Galician pharmaceutical Biofabri, from the Zendal group, has shown that its developed vaccine gives greater protection against the pathogen than the current vaccine. Biofabri successfully carried out the first clinical trials in humans in 2019 and plans for industrial production.
World Day to Fight Tuberculosis
The WHO stipulated that March 24 would be World Day to Fight Tuberculosis. It is commemorated that on March 24, 1882, Dr. Robert Koch announced the discovery of the tuberculosis bacillus.
In 1982, the first World Day to Fight Tuberculosis was held, sponsored by the World Health Organization (WHO) and the International Union Against Tuberculosis and Respiratory Diseases (UICTER). This event sought to educate the public about the devastating health and economic consequences caused by tuberculosis, its effect on developing countries, and its continuing tragic impact on global health.
Epidemiology around the world
According to the World Health Organization (WHO), nearly 2 billion people, one-third of the world's population, have been exposed to the tuberculosis pathogen. However, not all infections by M. tuberculosis causes tuberculosis and many infections are asymptomatic. Every year, eight million people get sick with tuberculosis, and two million people die from the disease worldwide. In 2004, about 14.6 million people had active disease with 9 million new cases. The annual incidence rate ranges from 356 per 100,000 in Africa and 41 per 100,000 in the Americas. It causes infectious diseases in women of reproductive age and is the leading cause of death among people with AIDS.
In 2005, the country with the highest estimated incidence of tuberculosis was Swaziland, with 1,262 cases per 100,000 people. India has the highest number of infections, with more than 1.8 million cases. In developed countries, tuberculosis is less common and is an urban disease. In the United Kingdom, the incidence of tuberculosis ranges from 40 per 100,000 in London, to less than 5 per 100,000 in rural areas of the south west of England, with the national average being 13 per 100,000. The highest rates of Western Europe are located in Portugal (31.1 per 100,000 in 2005) and Spain (20 per 100,000). These ranges compare to 113 per 100,000 in China and 64 per 100,000 in Brazil. In the United States, the overall rate of tuberculosis cases was 4.9 per 100,000 people in 2004. In Spain, tuberculosis remains endemic in some rural areas. The incidence of tuberculosis varies with age. In Africa, tuberculosis affects adolescents and young adults. However, in countries where tuberculosis has gone from high to low incidence, such as the United States, it is a disease of the elderly or the immunocompromised.
Infections, the rise of HIV and the neglect of tuberculosis control by programs have allowed its resurgence. The appearance of resistance in some strains has also contributed to a new epidemic, from 2000 to 2004, 20% of the cases of standard treatments were resistant to second-line drugs. The pace of new cases varies widely, even in neighboring countries, due to queues in health care systems.
A problem that is spreading in recent years is the appearance of M. tuberculosis resistant to antibiotics. Multidrug-resistant tuberculosis has been found in almost all the countries studied. In 2012, among the reported cases of pulmonary tuberculosis there were about 450,000 cases of multidrug-resistant tuberculosis. Almost 50% of them were from India, China and the Russian Federation. It is believed that 9.6% of MDR-TB cases had ultra-drug-resistant TB.
There are a number of factors that make people more susceptible to infection; the most important of these is HIV. HIV co-infection is a particular problem in sub-Saharan Africa, due to the high incidence of HIV in these countries. Smokers who consume more than 20 cigarettes a day also increase the risk of tuberculosis two to four times. Diabetes mellitus is a risk factor that is growing in importance in developing countries.
Other disease states that increase the risk of developing tuberculosis are Hodgkin lymphoma, end-of-kidney disease, chronic lung disease, malnutrition, and alcoholism.
Diet can also modulate risk. For example, among immigrants to London from the Indian subcontinent, Hindu vegetarians had an 8.5 times higher risk of tuberculosis, compared to Muslims who ate meat and fish every day. Although a causal relationship is not proven by these data this increased risk could be caused by micronutrient deficiencies, possibly iron, vitamin B12 or vitamin D.
Other studies have provided further evidence of a link between vitamin D deficiency and an increased risk of contracting tuberculosis. Severe malnutrition common in parts of the developing world leads to a greatly increased risk of developing active tuberculosis, due to its deleterious effects on the immune system. Along with overcrowding, poor diet can contribute to the strong link between TB and poverty.
Contenido relacionado
Digestive system
Human pregnancy
Brain stem
Toxoplasma gondii
Osteoblast