Testicle
The testicles are the male gonads, which produce sperm and the sex hormone (testosterone). They are the glandular organs that form the most important part of the male reproductive system. Its female equivalent would be the ovaries.
Anatomy of the testis
Macroscopic
- Location
The testicles, two in number, are found in the perineal region behind the base of the penis, inside the scrotal bag. They are surrounded by a set of bag-shaped covers, called the scrotum. The two gonads do not occupy the same level, since in most males the left testis descends a little more than the right. They are suspended from their lower end by the spermatic cord and are devoid of adhesions for most of their length. outer surface, so they are very mobile in all directions, being able to contract and ascend towards the inguinal ring.
- Number
There are two testicles, one on the right side and one on the left. Abnormally there can be only one testicle due to the absence of the development of the other, which when the epididymis and vas deferens are also missing, it is called monorchidism. When both testicles are missing it is called anorchidism.
- Size
In boys, the testicles are relatively small (2 to 3 cm long). At puberty they grow to be 4–8 centimeters (cm) in length and 2–4 cm in width. This size remains more or less similar throughout life, although a slight atrophy is sometimes noticed in old age or a slight increase in size due to steroid use. The excessive size of the testicles is due in most cases to a hydrocele (accumulation of fluid in the serous tunica of the testicle).
- Color, shape and consistency
The testicles are bluish-white, sometimes red when engorged with blood. This coloration is due to the bags that surround them. The testicle is ovoid in shape flattened transversely. It has a hard and somewhat elastic consistency due to the fibrous layer that surrounds it.
- Migration of the testicles
In humans, as in other mammals, the testicles come from inside the abdominal cavity, to the right and left of the lumbar spine, next to the kidneys. Towards the third month of fetal development, the testicles leave this region and descend through the inguinal canal, crossing the abdominal wall, dragging with it the bags that surround them to their final position. Incomplete descent of the testicle is called cryptorchidism.
Microscopic
From its surface, the testicle presents a testicular tunic
Seminiferous ducts
st Seminmal lobes.
vr= Right glasses.
rv= Go away.
Go! Efferent glass.
The seminiferous tubules are the place where sperm are produced. They are found within some lobes (there are about 380 per testicle) that have formed the testicular septa, which start from the tunica albuginea and join in the mediastinum testis . These lobules also contain interstitial tissue. Each "lobe" is estimated to contain 1-4 seminiferous tubules.
The seminiferous tubules empty through the straight tubules into cavities called the rete testis, in the mediastinum testis.
Auxiliary ducts
When the semen leaves the seminiferous ducts, it passes through:
- Testicular network, rete testis or network of Haller: inside the testicular mediastinum. It consists of three parts: septal rete or straight ducts, mediastinal rete and extratesticular rete, from which the efferent conductors are born.
- Efferent conductors: communicate the testis with the epididym.
- Epididym: narrow and elongated tube, located at the top of the testicle; connects the deferent ducts to the back of each testicle. It is made up of the meeting and the admonition of seminferous ducts.
Bags of the testicles
Anatomy
The testicles are surrounded by 7 layers that from surface to depth are:
- Scrotum: it is the skin that wraps the rest of testicular structures. It usually has hair with very deep hair follicles and abundant sebaceous glands.
- Darts: It is a fine muscle attached to the scrotum.
- Subcutaneous cell phone cap.
- External spermatic fascia.
- Cremoreter.
- Internal spermatic fascia.
- Vaginal tunic of the testicle.
Physiology
The bags keep the testicles at a temperature 1 to 3 °C below body temperature. This is related to the correct production of spermatozoa, since spermatid maturation (spermiogenesis) cannot occur at body temperature, since the enzymes involved in this process (β-polymerase and spermatogenic recombinase) need a lower temperature to carry out its function.
The scrotum is fat-free and its muscles react to heat by stretching or contracting the skin.
In addition, there is a temperature regulation mechanism dependent on the arterial system (which provides heat) and the venous system (which reduces temperature). All this means that when a man enters a medium whose temperature is below the ideal, the scrotum contracts in order to reduce the surface in contact with that medium and lose less heat, causing the size of the testicles to decrease.
Another curious fact is that there is a relationship between professions that involve sitting for a long time and suffering from infertility problems. When sitting, the testicles are closer to the body and their temperature rises, which can affect the spermatogenesis process.[citation needed]
Vascular supply of the testicles
- Arteries: the testicles are irrigated by the spermatic arteries, the deferential artery and the funicular artery.
- Veins: from the blood drain are entrusted the sperm veins. When they are obstructed they produce varicocele.
- Lymph vases.
The spermatic arteries divide forming a vascular tree up to the level of the microvessels, which are distributed among the seminiferous tubules, within the intertubular interstitial compartment. At this level the arterioles display locally regulated blood flow with regular rhythmic variations known as vasomotion, which are independent of the heartbeat.
Innervation
The testicles are innervated by the autonomic nervous system.
- Parasympathetic fibers, visceral and
- Sympathetic fibers that come from the testicular plexo.
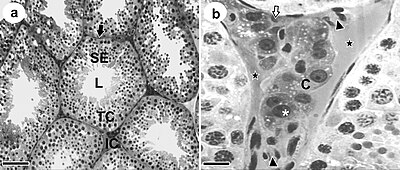
Cell types
In the testicle we can find three types of compartments, with different histological characteristics and of different embryonic origin: interstitial, tubular and tunic.
In the interstitial compartment
Leydig cells, macrophages, and microvessels of blood, lymphatics, and nerve fibers appear, surrounded by connective tissue#Loose connective tissue.
Leydig cells are derived from mesenchymal stromal cells. They are located outside the seminiferous tubules, respond to LH stimulation, and are involved in androgen synthesis.
In the tubular compartment
The seminiferous tubules are found, inside which the Sertoli cells (SC) are located. These cells come from the coelomic epithelium.
The SC are arranged in a basal compartment, surrounding the germ cells (spermatogonia) and in a luminal compartment, surrounding the spermatocytes and spermatids during their development.
SCs are closely linked to the sperm maturation process. They respond to FSH by producing androgen-binding protein (ABP) and inhibin.
In the robes
There are myoid cells, these cells are surrounding the seminiferous tubules. They perform a rhythmic contraction that causes peristaltic waves that help mobilize sperm and testicular fluids through the seminiferous tubules. This contractile activity is stimulated by oxytocin, serotonin, and prostaglandins. Likewise, these cells are involved in mediating the effects of hormones and growth factors on Sertoli cells and germ cells.
Functions of the testis
The testicle produces sperm and also hormones called androgens, among which is testosterone.
To produce spermatozoa, the process of spermatogenesis is carried out. This requires, in addition to germ cells, Sertoli cells, which constitute a support. There is a hematotesticular barrier that isolates the germinal epithelium from the rest of the organism so that there are no immunological reactions. Therefore, the Sertoli cells are responsible for carrying nutrients and excreting waste to the lumen from the germ cells.
For their part, the cells responsible for the manufacture of testosterone are the Leydig cells, which respond to FSH and LH (which are produced by the pituitary gland thanks to the action of GnRH from the hypothalamus) and produce testosterone in a pulsatile manner. The concentration of this hormone in the testicles is 500 times higher than that of the blood plasma.
Development of testicular function
The testicle begins to be hormonally active from the eighth week of gestation. Sertoli cells produce a substance that inhibits the Müllerian ducts when it is under the action of the hormone FSH (follicle-stimulating hormone). Said inhibitory substance is capable of inducing the regression of the aforementioned ducts, it has action in the abdominal phase of the descent of the male testicle and also produces an increase in the number of androgen receptors on the surface of the Leydig cells.
The complete development of the external genitalia in humans occurs between the 10th and 15th week of gestation. Said development is dependent on the enzymatic action of 5alpha-reductase, capable of producing dihydrotestosterone from testosterone. This enzyme product binds to androgen receptors within the sexual organs.
Diseases and disorders
- Anorquia: It is the absence of both testicles at birth.
- Criptorchydia: This is a disease that is characterized by failure in the decrease of the testicles from the abdominal cavity. During the fetal development process, the testicles are within that cavity, but thanks to the development they descend to the scrotum. The cryptorchid is remedied with surgery.
- Testicular cancer: occurs when abnormal cells within the testicles are divided and grow without control.
- Hydrocele: fluid accumulation in the scrotum. It's a benign disease.
Cultural use: Testicles
Sports
- In boxing, it is against the rules to glue under the belt, by the sensitivity to the pain of the testicles.
- In martial arts, violently beating this area as a vital point can cause intense inguinal pain and even death.
Graphic expression
- The testicles have been portrayed in colorful military drawings on the fuselage of warplanes.
- The testicles can be part of graffiti.
- They are commonly represented by two circles or ovals.
Vulgarisms
In a vulgar way, the testicles carry the connotations of laziness and laziness. In the Río de la Plata, the adjectives "boludo" and "pelotudo", for example, are synonymous with a stupid person, the latter with more pronounced connotations. Saying & # 34; is an egg-romper & # 34;, & # 34; is a ball-breaker & # 34;, refers to someone extremely annoying in the way he is. However, expressions like "boludo" or "güevón" (huevón, hueva) are also used to greet male friends or refer to them.
Linguistics
- The testicles have led to the creation of countless words [chuckles]Which one?] employed in argot and vulgar language, and therefore are an essential part of a repertoire of jokes.
- In a colloquial way, you can be known as "testis"or"the bass". Also the testicles are familiarly called: balls, balls, balls, coconuts, eggs, crotch or balls.
Music
- Songs have been written about the testicles and the scrotum.
- There are compact discs that in the title bear by name some part of the male player system.
- It is said that the size or absence of the testicles affect the tone of voice. (See also: Castrate).
Shaving
- It is usual to scrape the scrotum before surgical operations such as vasectomy or prostate extraction in case of almost oncological inflammation.
Gastronomy
- Cryadillas broth, instead of meat, meathead are used the testicles, wear onion, tomato, flavored with ground rocot.
- Slitting salt, dish similar to Lomo jumped, instead of loin meat, he's wearing rams, he's served with rice escort.
Witness
To act as a witness, the Hebrews had to hold their testicles, as a sign of the authenticity of their testimony; due to the idea that these organs were a sign of the nobility and honor of the male. Already in Christianity it was changed to the Crucifix or the Sign of the Cross.
Contenido relacionado
The New England Journal of Medicine
Come to
Transverse muscle of the nose