Stevens-Johnson syndrome
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are two forms of a life-threatening skin disease, in which cell death causes the epidermis separates from the dermis. The syndrome is believed to be a hypersensitivity complex that affects the skin and mucous membranes. Although most cases are idiopathic (cause unknown), the main confirmed cause is medication, followed by infections and, rarely, cancer.
History
The syndrome is named for Albert Mason Stevens and Frank Chambliss Johnson, American pediatricians who jointly published a description of the disorder in the American Journal of Diseases in 1922.
Genetics
In some East Asian (Han and Thai) populations studied, SJS induced by carbamazepine and phenytoin is closely related to HLA-B*1502 (HLA-B75), an HLA-B serotype of the broader HLA- serotype B15. A study in Europe suggested that the gene marker was only relevant to East Asians.
Based on findings from Asia, similar studies in Europe showed that 61% of patients with allopurinol-induced SJS/TEN had HLA-B58 (the frequency of the B*5801 allele phenotype in Europeans is normally of 3%). One study concluded: "...even when HLA-B alleles act as strong risk factors, in the case of allopurinol, they are neither sufficient nor necessary to explain the disease."
Causes
Stevens-Johnson syndrome is thought to stem from a disorder of the immune system. The immune reaction can be triggered by infections, drugs, or medications. In some groups, the drug reaction may be aggravated by genetic factors. Stevens-Johnson syndrome is 50% idiopathic. In the rest of the cases it can be an allergic reaction to one of the following factors:
- Virus (in particular herpes simple, Epstein-Barr virus, chickenpox virus, Coxsackie, ecovirus, and poliomyelitis virus)
- Bacterial infections (especially mycoplasms or Yersinia, brucellosis, diphtheria, tularemia, tuberculosis, and protozoa infections)
- Medications (especially sulfonamides, oxicames, penicillins, cephalosporins, macrolidos, triazoles, anticonvulsants and salicylates)
- Vaccines (diphtheria, typhus, BCG, oral polio vaccine)
- Hormonal changes in menstruation and malignant pregnancy
- Reactive arthritis
- Sarcoidosis.
Infections
Stevens-Johnson syndrome can be caused by infections. This usually includes common infections such as herpes simplex, influenza, mumps, cat scratch disease, histoplasmosis, Epstein-Barr virus, mycoplasma pneumoniae, or the like.
Medications/drugs
Although Stevens-Johnson syndrome can be caused by viral infections, malignancies, or severe allergic reactions to medication, the main cause appears to be the use of sulfa drugs and antibiotics.
SJS can be caused by adverse reaction to drugs such as allopurinol, phenytoin, valproic acid, levofloxacin, diclofenac, etravirine, isotretinoin, fluconazole, valdecoxib, sitagliptin, oseltamivir, penicillins, barbiturates, sulfonamide, azithromycin, oxcarbazepine, zonisamide, modafinil, lamotrigine, nevirapine, pyrimethamine, ibuprofen, ethosuximide, carbamazepine, nystatin, and anti-gout medications.
Medications traditionally known to induce Stevens-Johnson syndrome, erythema multiforme, and toxic epidermal necrolysis include sulfonamides, penicillins, barbiturates, lamotrigines, and phenytoin. The combination of lamotrigine with sodium valproate increases the risk of suffering from the syndrome. Nonsteroidal anti-inflammatory drugs are a rare cause of SJS in adults; the risk is highest for older patients, women, and those starting treatment. Typically, drug-induced symptoms of SJS emerge within a week of starting medication. People with lupus or HIV infections are more susceptible to drug-induced SJS.
SJS can also be caused by cocaine use.
Epidemiology
Stevens-Johnson syndrome is a rare condition, with a reported incidence of around 2.6 to 6.1 cases per million people per year. In the United States, there are approximately 300 new diagnoses per year. The condition is most common in children and young adults. Males are more affected than females, with cases occurring at a ratio of two to one (2:1).
Clinic
Risk factors
Risk factors are a previous history of erythema multiforme or Stevens-Johnson.
Symptoms
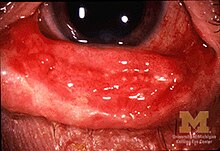
The syndrome is characterized by a sudden and progressive development of a pleomorphic rash with vesicles and bullae on the skin and mucous membranes. It usually begins with a fever of 39 to 40 °C, severe headache, sore throat, and fatigue, which is misdiagnosed and therefore mistreated with antibiotics. Nikolsky's sign is negative in most cases. Ulcers and other lesions begin to appear on the mucosa, almost always in the mouth and lips, but also in the genital and anal regions. Those that appear in the mouth are usually extremely painful and reduce the patient's ability to eat or drink. Conjunctivitis occurs in approximately 30% of children who develop SJS. An outbreak of round wounds about one inch in size arises on the face, trunk, arms and legs, and the soles of the feet, but usually not on the scalp.
In the most severe cases, electrolyte balance disturbances, tachypnea and dyspnea, hematuria, albuminuria, cardiac arrhythmias, pericarditis, congestive heart failure, stupor, and coma may occur.
Pathology
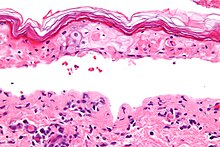
The syndrome, like toxic epidermal necrolysis and erythema multiforme, is characterized by confluent epidermal necrosis with minimal associated inflammation. Acuity is evident by looking at the pattern of the horny layer.
Differential diagnosis
It must be differentiated from: bullous impetigo, pemphigus vulgaris, septicemia, pemphigoid, collagen vascular disease, meningococcemia, Behçet's syndrome. Bacteriological cultures of suspected sources of infection should be done.
From a pathological point of view, the most characteristic finding is epidermal necrolysis, spongiosis, intracellular edema, vacuolar changes at the dermal-epidermal junction, edema, and extravasation of erythrocytes. Skin biopsy can confirm the diagnosis.
Classification
There is a consensus in the specialized medical literature that Stevens-Johnson syndrome is considered a milder form of toxic epidermal necrolysis (TEN). These conditions were first recognized in 1922. Both diseases can be confused with erythema multiforme. Erythema multiforme is sometimes caused by a reaction to medication, but is more often a type III hypersensitivity reaction to infection (often caused by herpes simplex) and is relatively benign. Although both SJS and NET can also be caused by infections, they are more often the adverse effects of medications. Its consequences are potentially more dangerous than those of erythema multiforme.
Treatment
SJS is a dermatologic emergency.
He must be hospitalized for continuous monitoring and management of complications that arise.
All medications should be discontinued, particularly those known to cause SJS reactions. Patients with documented mycoplasma infections may be treated with oral macrolides or oral doxycycline.
Initially, treatment is similar to this for burn patients and ongoing care may only be supportive (eg intravenous therapy and nasogastric tube or parenteral nutrition) and symptomatic (eg analgesic mouth rinse for ulcer oral). Sometimes skin lesions require opioid analgesia. To relieve burning pain in the oral cavity, rinse with warm saline or diphenhydramine solution. Conjunctivitis can be treated with lidocaine. An anesthetic cream such as EMLA can be used on mucous membranes.
An ophthalmologist should be consulted immediately, as SJS often causes scar tissue to form within the eyelids, leading to vascularization of the cornea, compromised vision, and a host of other eye problems.
Dermatologists and surgeons tend to disagree on whether the skin should be debrided.
Beyond this kind of supportive care, there is no accepted treatment for SJS. Treatment with corticosteroids is controversial. Recent retrospective studies suggested that corticosteroids increase hospital stays and complication rates. There is no corticosteroid test for SJS and it can be managed satisfactorily without them.
Other agents have been used, including cyclophosphamide and cyclosporine, but none have shown much therapeutic success. Treatment with intravenous immunoglobulin (IVIG) has shown some progress in reducing the length of the reaction and improving symptoms. Other common supportive measures include the use of anesthetics and antiseptics for pain management, maintaining a warm environment, and intravenous pain relievers.
Forecast
SJS itself (with less than 10% of the body surface area involved) has a mortality rate of about 5%. The risk of death is estimated using the SCORTEN scale, which takes a number of prognostic indicators into consideration. Other consequences may be organ failure or damage, corneal tearing, and blindness.
Most common complications
- Dry eye syndrome
- Photophobia
- Ceguera
- Sepsis (systematic inflammatory response syndrome)
- Post-traumatic Stress Syndrome
The most common are secondary infections and pulmonary complications. Dehydration and electrolyte disturbances, acute tubular necrosis, ophthalmic complications, and arrhythmias have also been reported. Death occurs in 5 to 15% of cases without treat. The risk of recurrence is 37% or more.
Notable cases
- Padma Lakshmi, actress, model, celebrity and cookbook writer.
- Manute Bol, a professional basketball player and a member of the NBA Washington Bullets teams, Golden State Warriors, Philadelphia 76ers and Miami Heat, who died from the complications of the syndrome.
Contenido relacionado
Epididymis
Sarcoma
Medical diagnostic