Spinal cord
The spinal cord is a long cylindrical structure, slightly flattened in an anteroposterior direction, located in the vertebral canal and is responsible for transmitting nerve impulses to the thirty-one pairs of spinal nerves, connecting the brain. with the body, through two basic functions: the afferent, in which sensations from the trunk, neck and the four extremities towards the brain are called, and the efferent, in which the brain orders the effector organs to carry out a certain action, carrying these impulses to the trunk, neck and limbs.
External Anatomy
The spinal cord is considered to be the largest nervous tissue in the human body; the axons of its neurons can be up to a meter long. Weighing approximately 30 grams, in its full development the spinal cord reaches a length of 45 cm in males and 42 cm in females within the intravertebral bone called the spinal canal in the archial media, in the middle archial part of the atlas to the first or second lumbar vertebra. In effect, in the newborn the marrow reaches the lumbar 3, two vertebrae below, and embryonically it reaches the base of the coccyx.
It is cylindrical in shape in the upper cervical and lumbar segments, while ovoid with a transverse diameter greater than the obverse in the lower cervical and thoracic segments. The medulla is asymmetric in almost 80% of humans, with the right side being the largest in 75% of asymmetries. Such asymmetry is due to the presence of more descending corticospinal tract fibers on the larger side.
The spinal cord has two faces and two edges: an anterior face, two lateral edges, and a posterior face. The anterior aspect in the midline presents the anterior median sulcus and is limited laterally by the anterior collateral sulci, which are the apparent origins of the motor or efferent nerve roots of the spinal nerves and that also separate it from the lateral aspects. The posterior face presents a posterior median groove that is extended by a septum to the central gray matter and bordered on the sides by posterior collateral grooves that correspond to the apparent origins of the sensory or afferent nerve roots of the spinal nerves; between them there is a groove called the paramedian that superficially divides the medulla into two parts that correspond to the Goll and Burdach bundles (Gracile and Cuneiform fasciculus respectively).
There are two thickenings, one cervical and the other lumbosacral:
- cervical intumence: 'C4' to 'T1' this thickening is due to the nerve roots that will transmit sensitivity and motor action to and from the superior members (brazo, antebrazo and hand).
- lumbosacra intumescence: 'L1' to the 'S3' is due to the nerve roots that allow to transmit the sensitivity and motor action to and from the lower members (museum, leg and foot).
In its lower portion it thins rapidly and then ends at the tip of a cone known as the terminal cone. On the lateral parts, it is attached to the dentate ligaments and on the lower part it is continuous with the filum terminale that extends to the bottom of the dural sac at the level of the second sacral vertebra; and that in addition the coccygeal ligament that is inserted in the anterior face of the coccyx continues to be formed.
Three membranes concentrically surround the spinal cord: the pia mater, the arachnoid mater, and the dura mater. The pia mater is the one that directly surrounds it and enters the grooves. Above it and related to a loose part of the arachnoid we find a space filled with cerebrospinal fluid called the subarachnoid space. Above this space is the most homogeneous and distinguishable part of the arachnoid. It is like a fine, transparent and loose network that cannot be introduced into the grooves of the medulla. In some parts it is difficult to differentiate the pia mater from the arachnoid mater. For this reason, we sometimes use the term pia-arachnoid. Finally, we have the dura mater, which is the outermost, fibrous, and strong meningeal layer. Between the arachnoid mater and the dura there is a virtual space in normal states but important in pathological states called the subdural space.
The spinal cord is attached to the medulla oblongata above with its continuity with the medulla, in its middle part by means of conjunctive processes to adhere to the dura mater, fins on the nerve roots as dependencies of the pia mater, both constituting types of extensions the dentate ligaments. At the lower end by a prolongation of the dura mater that surrounds the filum terminale, fixing to the base of the coccyx.
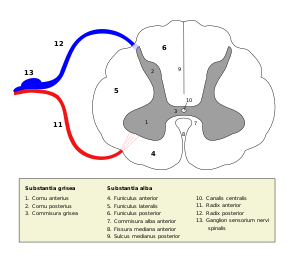
Internal anatomy
In a cross section, the medulla is made up of a gray area along its entire length and in its divisions, the grey matter in the shape of an "H" or butterfly in the center and a peripheral white matter, unlike in the brain. The relatively slender posterior processes that almost reach the posterior groove are called the posterior horns; the broad, rounded anterior processes are called anterior horns. The three-dimensional arrangement of the anterior and posterior horns make up true columns that run through the spinal cord to form the anterior and posterior gray columns. The posterior horns, functionally somatosensory, are formed by sensory neurons that receive impulses arriving from the posterior roots. The anterior horns, functionally somatomotor, are made up of motor neurons whose axons exit through the anterior roots. In the upper thoracic and lumbar segments there is a small lateral horn that emerges from the junction of the anterior horn with the posterior horn and contains sympathetic visceral neurons. In the lateral part of the base of the posterior horn of the upper cervical segments, it is difficult to distinguish the boundary between the gray matter and the white matter because cells and nerve fibers are mixed: it is the reticular formation that it continues superiorly as the reticular formation of the brainstem.
Their halves are divided into three and are divided sagittally by two processes: on the dorsal side we find the posterior median septum, long and narrow, and ventrally the anterior median fissure , which is broader and shorter. It is divided longitudinally into 31 segments, one for each pair of nerves; Thus, the spinal nerves are located in eight cervical, twelve thoracic, five lumbar, five sacral, and one coccygeal nerve. Each segment has two pairs of roots (dorsal and ventral) located symmetrically on the dorsal and ventral side.
The grey matter is composed mainly of cell bodies and supporting cells (neuroglia). It has two anterior gray horns and two posterior gray horns joined by the grey commissure. This gray commissure is divided into a posterior and anterior part by a small central hole called the ependymal canal or medullary ependyma, this being a vestige of the primitive neural tube. At the thoracic and lumbar level, the wedge-shaped lateral gray horns also appear, corresponding to the somas of the neurons that form the sympathetic or thoracolumbar autonomous system. Its consistency is rather uniform, although the substance surrounding the ependymal duct is more transparent and soft, which is why it has been given the name central gelatinous substance.
The white matter of the medulla is the one that surrounds the gray matter and is made up mainly of fascicles or bundles of fibers, becoming the axons that carry information. It is divided into three basic regions that are the anterior, lateral and posterior, in image 4, 5 and 6, respectively.
The dorsal root entry site is marked by the dorsolateral groove; Likewise, the entrance of the ventral root is marked by the ventrolateral groove. These references divide the white matter into a dorsal funiculus, one between the sulci, called the lateral funiculus, and a ventral funiculus, while further dividing into the cervical and upper thoracic segments, the dorsal funiculus is divided by the medial dorsal sulcus. in the cuneiform fasciculus, the most lateral, and the gracile fasciculus.
Histology
In the spinal cord we can also find certain types of cells that serve as support, such as ependymal cells, elongated cells that have two extensions, which emit towards the anterior or posterior medial sulcus where they constitute the anterior ependymal cone and the later. We also found neuroglial cells, from the same origin as the ependymal cells, only without their primitive extensions. They are found scattered in the gray matter as in the white.
Gray Matter
- Asta dorsal: The asta posterior receives axons of the dorsal nodes through the homonymous roots and contains sensitive beams. Understand the core of the Clarke column where they make sinapsis the fibers that transmit deep unconscious sensitivity, the of Rolando where synapses the fibers that transmit the thermo-algeic sensitivity and the own core where synapses the fibers that transmit protopathic touch sensitivity or thick touch.
- Interlateral assault: It is only found in the upper thoracic and lumbar segments (L1, L2 and sometimes L3) of the marrow. It contains sympathetic preganglionar neurons. It also has in the S2-S3-S4 parasympathetic nuclei that will form part of the pelvic or erector splenic nerve of Eckhard that grants the parasympathetic continent in the region of the lower hypogastric plexus.
- Ventral asta: or above, it consists of axons of multi-polar motor neurons. Understand the antero-external core inervading the higher and lower members and the antero-intern core destined for the dorsal muscles of the trunk and neck. The central nucleus presents a portion in C1-C2 that corresponds to the spinal roots of the spinal nerve or accessory or 11° cranial nerve (inerva to the trapeze and the esternocleidomastoid) its portion of C3-C4-C5 then gives rise to the phrenic nerve that must inerve the diaphragm.
- Intermediate area: contains a large number of interneurons.
White matter
The white matter of the spinal cord is made up of a large number of nerve fibers, neuroglia, and blood vessels. In a cross section, its arrangement around the gray matter is observed. Its color is due to the presence of a large proportion of longitudinally running myelinated fibers, although there is also a certain amount of unmyelinated fibers. The nerve fibers of the white matter are responsible for joining the spinal cord segments with each other, and the spinal cord with the brain.
- Lateral cord: They are sensitive ascending pathways whose neuronal bodies are found in the dorsal nodes and participates in two modes conscious perception: cinemas (pressure and vibration) and discriminatory tact o epicritic touch (difference of two points, recognition of forms). It consists of two beams or fascicles (since pairs both), the Goll beam medially and immediately lateral the Burdach beam. It has small motor fibers, which take care of reflex arches: among the Goll beams, is the septomarginalbetween the Goll and the Burdach, the semi-lunar fascicle.
- Side cord: Contains upward paths as descendants. The ascendants are responsible for carrying stimuli of pain, temperature and thick touch or protopathic touch, and are composed of several fascicles: the That's great., the espinotal, the espinoreticular and espinotectal. Instead the descending fibers are motors, they are responsible for the control of voluntary movements and are the following fascicles: corticospinal, headings and reticulospine.
- Previous cord: Contains upward paths as descendants. The ascendants are three fascicles, each in charge of different information: the espinotectal takes care of movements reflections of eyes and head when visual information comes, espinoolivar sends information to the cerebellum of the skin feeling and the ventral thortamic carries thick touch and pressure. The motors are responsible for movement control and are the following fascicles: reticulospinal medial, vestibulospinal and anterior corticospinal.
Spinal cord injuries
Spinal cord injury, or myelopathy, causes one or more of the following symptoms:
- Paralysis in trunk, neck and limb muscles.
- Loss of trunk sensitivity, neck and extremities
- Disorders (discontrol) of bladder, anal or seminal sphincter.
- Block of the sympathetic system (hypotension, bradycardia, abdominal strain).
The degree of involvement depends on the degree of damage: it can be a complete lesion (if all the indicated symptoms-signs are observed) or an incomplete lesion if It only presents some of the symptoms or all but partially (for example, partial and not total paralysis).
Level of injury: In the clinic it is very important to know the level of the spinal cord affected. In order to understand the relationship between the affected medullary segment and the level of paralysis produced, it must be remembered that bone, unlike nerve cells, have growth after the development of what is the nerve tube or marrow, more important than any bibliographical reference. that supports this outline is the clinical reference.
Clinical reference: The damage of the 'C4' to 'C7' causes paralysis that includes the four extremities, the affectation at the level of "T11" causes paralysis of the lower extremities. In order to understand the level of the lesion and the damage caused, it is necessary to take into account the gap in the speed of development between the Nervous System and the bone part, which is reflected in a growing gap between sensory levels and real levels; that is, the territory of S1 will topographically belong to the sensory root of about two higher levels, leaving the roots of the medulla in T12 and descending to reach the corresponding dermatome.
Pathology: Bone damage will compress different roots of the spinal cord. Good postural hygiene is necessary to avoid long-term complications; Even so, many of these alterations have a genetic basis or are caused by accidents that are difficult to prevent. You can turn to a spinal cord specialist.
Treatment: Vertebrospinal cord injury, when it is complete, requires surgical fixation of the spine performed by a specialized surgical professional; if the lesion affects only the bone, the intervention can be successful; If the nerve is damaged, or is damaged in the intervention, it will be very important to assess self-care deficits and develop a comprehensive care plan usually designed by nursing professionals and that will cover other disciplines, both health as social.
In the body, the central nervous system is represented solely by the brain. The spinal cord, which is an extension of the brain, is responsible for carrying nerve impulses.
Contenido relacionado
Rhodopsin
Parapholis
Magnolia