Progesterone
Progesterone, also known as P4 or pregn-4-en-3,20- dione, is a C-21 steroid hormone involved in the female menstrual cycle, pregnancy (it promotes gestation) and embryogenesis, both in humans and other species. Progesterone belongs to a class of hormones called progestogens, and is the main naturally occurring human progestogen. Its main source is the ovary (corpus luteum) and placenta, although it can also be synthesized in the adrenal glands and in the liver.
Progesterone is one of the sex hormones that develops at puberty and adolescence in females, and it acts mainly during the second part of the menstrual cycle, stopping the endometrial changes induced by estrogens and stimulating maturational changes., thus preparing the endometrium for embryo implantation. Progesterone is also responsible for thickening and holding the endometrium in the uterus: when its concentration decreases, the endometrium is shed, producing menstruation. It is the hormone responsible for the development of secondary sexual characteristics in a woman, and serves to maintain pregnancy.
In addition to exercising its function in the endometrium, this hormone acts in other tissues such as the breasts, producing breast tension. This is due to the increase in the size of the mammary glands. It also acts at the digestive level, its muscle relaxant effect can lead to diarrhea. It is precisely this muscle-relaxing effect that prevents the uterus from contracting, favoring embryo implantation. Another of the consequences of muscle relaxation is the feeling of tiredness and drowsiness. All these symptoms are usually associated with the period of menstruation, since in this phase of the cycle progesterone levels are higher.
Chemistry and discovery
Progesterone was independently discovered by four research groups.
Willard Myron Allen co-discovered progesterone with his professor of anatomy George Washington Corner at the University of Rochester School of Medicine in 1933. Allen first determined its melting point, molecular weight, and partial molecular structure. He also gave it the name progesterone derived from progestational steroidal ketone.
Like other steroids, the structure of progesterone consists of four interconnected cyclic hydrocarbons, with ketone and oxygen functional groups, as well as two methyl substituents.
Fonts
Animals
Progesterone is produced in the ovaries (more specifically in the corpus luteum after ovulation), in the adrenal glands (near the kidney), and, during pregnancy, in the placenta. Progesterone is also stored in adipose tissue (fat).
In humans, increasing amounts of progesterone are produced during pregnancy:
- At first, the source is the luteum body that has been "rescued" by the presence of human chorionic gonadotropin (hCG) of the embryo.
- However, after the 8th week progesterone production moves to the placenta. Placenta uses maternal cholesterol as an initial substrate and most of the progesterone produced penetrates to maternal circulation, but a part is collected by fetal circulation and used as a substrate to synthesize fetal corticosteroids. At the end of pregnancy, the placenta produces about 250 mg per day of progesterone.
- An additional source of progesterone are dairy products. Dairy products contain a lot of progesterone, because in dairy farms the pregnanted cows are milked, when the milk progesterone content is high. After the consumption of dairy products the level of bioavailable progesterone increases.
Plants
Progesterone has been detected in at least one plant, Juglans regia. In addition, progesterone-like steroids are found in Dioscorea mexicana, a plant in the family of yams, native to Mexico. It contains a steroid called diosgenin, which is taken from the plant and converted to progesterone. Diosgenin and progesterone can also be found in other species of Dioscorea.
Another plant that contains substances easily convertible to progesterone is Dioscorea pseudojaponica, native to Taiwan. Some research has shown that Taiwanese yam contains saponins, a steroid that can be converted to diosgenin and then to progesterone.
Many other Dioscorea species of the yam family contain steroidal substances that could give rise to progesterone. Among the most notable are Dioscorea villosa and Dioscorea polygonoides. One study showed that Dioscorea villosa contains 3.5% diosgenin. Dioscorea polygonoides has been found to contain 2.64% diosgenin, shown by chromatography gas-mass spectrometry. Many of the Dioscorea species originating from the yam family grow in countries with tropical and subtropical climates.
Summary
Biosynthesis
In mammals, progesterone (6), like all steroid hormones, is synthesized from pregnenolone (3), which in turn derives cholesterol (1) (see top of figure on the right).
Cholesterol (1) undergoes double oxidation to produce 20,22-hydroxycholesterol (2). This vicinal diol is then oxidized with loss of the side chain beginning at position C-22, producing pregnenolone (3). This reaction is catalyzed by cytochrome P450scc. The conversion of pregnenolone to progesterone takes place in two steps. First, the 3-hydroxyl group is oxidized to a ketone (4) and second, the double bond isomerized from C-5 to C-4, via a catalyzed ketone/enol tautomerization reaction. by 3beta-hydroxysteroid dehydrogenase.
Progesterone (see lower half of the figure to the right) is in turn the precursor of the mineralocorticoid aldosterone and, after its conversion to 17-hydroxyprogesterone (another natural progestogen), of cortisol and androstenedione. Androstenedione can be converted to testosterone and estrone.
Pregnenolone and progesterone can also be synthesized by yeast.
Laboratory synthesis
In 1940, Russell Marker developed for the pharmaceutical company Parke-Davis an inexpensive process for the semisynthesis of progesterone from the steroid diosgenin isolated from yams (see figure to the right). This synthesis is known as the degradation from Marker. Several additional semi-synthesises of progesterone from various steroids have also been reported. For example, cortisone can be simultaneously deoxygenated at the C-17 and C-21 positions by treatment with iodotrimethylsilane in chloroform to produce 11-keto-progesterone (ketogestin), which in turn can be reduced at the 11-position to obtain progesterone.
In 1971, William Summer Johnson achieved a total synthesis of progesterone (see figure to the right). The synthesis begins by reacting the phosphonium salt 7 with phenyllithium to produce a ylide of phosphonium 8. The ylide 8 is reacted with an aldehyde to produce the alkene 9. The ketal protecting groups of 9 hydrolyze to produce the diketone 10, which in turn cyclizes to form the cyclopentenone 11. The 11 ketone is reacted with methyl lithium to obtain the tertiary alcohol 12, which in turn is treated with acid to produce the tertiary cation 13. The key step in the synthesis is the cation-π cyclization of 13 in which the B, C and D rings of the steroids are formed simultaneously to produce 14. This step resembles the cationic cyclization reaction used in steroid biosynthesis and is therefore known as biomimetic. In the next step the enol orthoester is hydrolyzed to produce the ketone 15. The cyclopentene A-ring is then opened by oxidation with ozone to produce 16. Finally, the diketone 17 undergoes intramolecular aldol condensation by treatment with aqueous potassium hydroxide to produce progesterone.
Concentration
In women, the concentration of progesterone is relatively low during the preovulatory phase of the menstrual cycle, rises after ovulation, and remains elevated during the luteal phase, as shown in the diagram. The progesterone concentration tends to be 5 ng/ml after ovulation. In pregnancy, the concentration of progesterone is initially maintained at luteal values. With the beginning of the luteal-placental change in pregnancy, the concentration begins to rise and can reach 100 or 200 ng/ml at the end of the pregnancy. Whether or not a decrease in progesterone is essential for the initiation of parturition has been debated and this may be different between species. After childbirth and during lactation the concentration of progesterone is very low.
Progesterone concentration is relatively low in children and in postmenopausal women. Adult males show values similar to those in the follicular phase of the menstrual cycle in females.

- The marked intervals By biological stage (by biological stages) can be occupied in menstrual cycles in close follow-up with regard to other indicators of their biological progress, with the time scale compressed or stretched depending on how fast or slow, respectively, is the progress of the cycle compared to an average cycle.
- Labeled intervals Inter-cycle variability (inter-cycle variation) are more appropriate to be used in unmonitored cycles where only the beginning of the cycle is known and women know the average duration of their cycle and ovulation time, and are relatively regular, with the time scale compressed or stretched depending on how short or long, respectively, be the cycle compared to the average population.
- The marked intervals Inter-woman variability (variability among women) are more appropriate to be used when ovulation duration and time are unknown and only the beginning of the cycle is known.
| Circumstances | Reference intervals for blood analysis | ||
|---|---|---|---|
| Lower limit | Higher limit | Units | |
| Female with menstrual cycle | (see diagram) | ||
| Postmenopausal female | ≤2. | 1 | ng/mL |
| 6 | 3 | nmol/L | |
| Female taking oral contraceptives | 0.34 | 0.92 | ng/mL |
| 1.1. | 2.9 | nmol/L | |
| 16-year-old male or older | 0.27 | 0.9 | ng/mL |
| 0.86 | 2.9 | nmol/L | |
| Female or male between 1 and 9 years | 0.1 | 4.1 or 4.5 | ng/mL |
| 0.3 | 13 | nmol/L | |
Effects
Progesterone exerts its main action through the intracellular progesterone receptor, although there is also a membrane-bound receptor called PGRMC1, which is responsible for various fertility disorders, although it is still not very widespread. In addition, the Progesterone is a very potent antagonist of the mineralocorticoid receptor (the receptor for aldosterone and other mineralocorticoids). Progesterone prevents the activation of mineralocorticoid receptors by binding to these receptors with an affinity that exceeds even that of aldosterone and other corticosteroids, such as cortisol and corticosterone.
Progesterone has a number of physiological effects that are amplified in the presence of estrogen. Estrogens via estrogen receptors upregulate progesterone receptor gene expression. Also, elevated levels of progesterone strongly reduce the sodium-retaining activity of aldosterone, resulting in natriuresis and a reduction in fluid volume. extracellular. On the other hand, progesterone withdrawal is associated with a temporary increase in sodium retention (reduced natriuresis, with an increase in extracellular fluid volume) due to the compensatory increase in aldosterone production, which counteracts the blockade of progesterone. mineralocorticoid receptors by previously elevated levels of progesterone.
Reproductive system
Progesterone has key effects via non-genomic signaling in human sperm as they migrate through the female tract before fertilization occurs, although the receptors have not yet been identified. Detailed characterization of the events that that occur in sperm in response to progesterone has elucidated certain events, including intracellular calcium transits and sustained changes, slow calcium oscillations, now thought to possibly regulate motility. Interestingly, progesterone has also been shown to produce effects on sperm. octopus sperm.
Progesterone modulates the activity of sperm cation channels (CatSper) Ca2+. Since eggs release progesterone, the sperm could use progesterone as a homing signal to swim toward the egg (chemotaxis). Therefore, substances that block the progesterone binding site in CatSper channels could be used in male contraception.
Progesterone is sometimes called the "pregnancy hormone," and has many functions related to the development of the fetus:
- Progesterone converts endometrial to its phase of secretion to prepare the uterus for its implantation. At the same time progesterone affects the vaginal epithelium and cervical mucus, making it thick and impenetrable for sperm. If a pregnancy does not occur, progesterone levels decrease, giving rise to menstruation in the human. Normal menstrual bleeding is due to the abstinence of progesterone. If an ovulation does not occur and the luteum body does not develop, progesterone levels may be low, leading to abnormal dysfunctional uterine bleeding.
- During implantation and gestation, progesterone seems to reduce maternal immune response to allow acceptance of pregnancy.
- Progesterone decreases the contractility of the uterine smooth muscle.
- A fall in progesterone levels is, possibly, a step that facilitates the beginning of childbirth.
The fetus metabolizes placental progesterone into the production of adrenal steroids.
Nervous system
Progesterone, like pregnenolone and dehydroepiandrosterone, belongs to the group of neurosteroids. It can be synthesized within the central nervous system and also serves as a precursor to another important neurosteroid, allopregnanolone.
Neurosteroids affect synapse function, are neuroprotective, and affect myelination. They are being investigated for their potential to improve memory and cognitive ability. Progesterone affects the regulation of apoptotic genes.
Its effects as a neurosteroid work predominantly through the GSK-3 beta pathway, as an inhibitor. (Other GSK-3 beta inhibitors include bipolar mood stabilizers, lithium, and valproic acid.)
Other effects
- It elevates the levels of the epidermal growth factor, a factor that is often used to induce proliferation, and is used to maintain stem cell cultures.
- Increases the central temperature (thermogenic function) during ovulation.
- Reduce spasms and relax smooth muscles. The bronchus is extended and the mucous is regulated. (Progesterone receptors are widely present in submucosal tissue.)
- It acts as an anti-inflammatory agent and regulates the immune response.
- Reduces the activity of the gallbladder.
- It may affect the health of gums, increasing the risk of gingivitis and tooth decay.
- It seems to avoid endometrial cancer by regulating the effects of estrogen.
Adverse effects
Progesterone in pill form (actually a synthetic version, like a progestogen) taken at 400 mg as cited by the patent can cause increased fluid retention, which can result in epilepsy, migraine, asthma, kidney dysfunction or cardiac. Blood clots can develop that can cause strokes and heart attacks, which can lead to death or long-term disability; Pulmonary embolism or breast cancer may also develop as a result of progesterone treatment. Progesterone is associated with an increased risk of thrombotic diseases, such as thrombophlebitis, cerebrovascular disease, pulmonary embolism, and retinal thrombosis.
Common adverse effects include cramps, abdominal pain, bone pain, perineal pain, headache, arthralgia, constipation, dyspareunia, nocturia, diarrhoea, nausea, vomiting, breast enlargement, joint pain, flatulence, hot flushes, decreased libido, thirst, increased appetite, nervousness, drowsiness, excessive urination at night. Psychiatric effects include depression, mood swings, emotional instability, aggression, abnormal crying, insomnia, forgetfulness, sleep disorders.
Less common side effects that may occur include allergies, anemia, swelling, fatigue, tremor, urticaria, pain, conjunctivitis, dizziness, vomiting, myalgia, back pain, breast pain, genital itching, genital yeast infection, upper respiratory tract infection, cystitis, dysuria, asthenia, xerophthalmia, syncope, dysmenorrhea, premenstrual tension, gastritis, urinary tract infection, vaginal discharge, pharyngitis, sweating, hyperventilation, vaginal dryness, dyspnea, fever, edema, flu symptoms, dry mouth, rhinitis, leg pain, skin discoloration, skin disorders, seborrhea, sinusitis, acne.
Current research suggests that progesterone plays an important role in signaling insulin release and pancreatic function, and could affect susceptibility to diabetes. Women with high levels of progesterone during pregnancy have been shown to are more likely to develop glucose abnormalities.
Medical applications
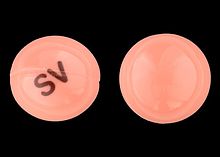
The use of progesterone and its analogues have many medical applications, both in coping with critical situations and in coping with long-term decline in natural progesterone levels. Due to the low bioavailability of oral progesterone, many synthetic progestogens have been designed with improved oral bioavailability. Progesterone was approved by the United States FDA as a vaginal gel on July 31, 1997, in capsule form. orally on May 14, 1998, by injection on April 25, 2001, and as a vaginal insert on June 21, 2007. In Italy and Spain, progesterone is sold under the brand name Progeffik.
Bioavailability
The route of administration affects the effect of the drug. Orally, progesterone has a wide range in variability in absorption and bioavailability from person to person, whereas synthetic progestogens are rapidly absorbed, have a longer half-life than progesterone, and maintain stable blood levels.
Progesterone does not dissolve in water and is not well absorbed by mouth unless it is micronized in oil. Progesterone products are often sold as capsules containing micronized progesterone in oil. Progesterone can also be administered via vaginal or rectal suppositories or pessaries, transdermally via gels or creams, or via injection (although the latter has a short half-life requiring daily administration).
"Natural Progesterone" Yam derivatives do not require a prescription, but there is no evidence that the human body can convert their active ingredient (diosgenin, the plant steroid that is chemically converted to produce progesterone industrially) into progesterone.
Specific uses
- Progesterone is used to keep pregnancy in cycles of Assisted Reproduction Technology (TRA) such as In-vitro Fertilization (IVF). While the daily intramuscular injections of progesterone in oil (PIO) have been the standard administration route, PIO injections are not approved by FDA for use in pregnancy. A recent meta-analysis showed that the intravaginal pathway with a dose and frequency of the proper dose is equivalent to daily intramuscular injections. In addition, a recent study of concordance cases comparing vaginal progesterone with PIO injections showed that live birth rates were almost identical with both methods.
- Progesterone is used to control persistent anovulatory bleeding. It is also used to prepare the lining of the uterus in sterility therapies and to keep the pregnancy early. Patients with recurrent pregnancy loss due to inadequate progesterone production could receive progesterone.
- Progesterone is also used in non-pregnant women with a menstruation delay of one or more weeks, so that the engrossed endomerium is unlearned. This process is called a deprivation bleeding of progesterone. Progesterone is taken by mouth for a short period of time (usually a week), then progesterone is suspended and bleeding should occur.
- Progesterone is being investigated as potentially beneficial in the treatment of multiple sclerosis, as the characteristic deterioration of nerve myelin stops during pregnancy. When progesterone levels rise; deterioration begins again when levels drop.
- Vaginal progesterone is being investigated as potentially beneficial in the prevention of premature births in women at risk of premature birth. The initial study by Fonseca suggested that vaginal progesterone could prevent premature delivery in women with a premature birth history. According to a recent study, women with a short cervix who received hormonal treatment with a progesterone gel had a reduction in the risk of giving birth before time. Hormonal treatment was given every day during the second half of pregnancy.
A later, larger study showed that vaginal progesterone was no better than placebo in preventing recurrent preterm birth in women with a history of prior preterm birth, but a planned secondary analysis of the data from this trial showed that women with a short cervix at baseline in the trial had two advantages: reducing the number of deliveries less than 32 weeks and reducing the frequency and time their babies were in intensive care. In another trial, progesterone vaginalis was shown to be better than placebo in preventing preterm birth before 34 weeks in women with an extremely short neck at baseline. An editorial by Roberto Romero discusses the role of ultrasound cervical length in patient identification who might benefit from progesterone treatment.
- Progesterone also has a role in skin elasticity and bone resistance, in cellular breathing, in nerve tissue and in female sexuality, and the presence of progesterone receptors in certain muscle and fatty tissues could give a clue to the role of these in sexual dimorphism.
- Progesterone receptor antagonists, or selective progesterone receptor modulators (SPRMs), such as the RU-486 (Mifepristona), can be used to prevent conception or induce medical abortion.
Note that hormonal methods of birth control do not contain progesterone, but rather a progestin.
Progesterone may affect male behavior.
Progesterone is beginning to be used in the treatment of the skin disease hidradenitis suppurativa.
Brain Damage
Previous studies have shown that progesterone supports the normal development of neurons in the brain, and that the hormone has a protective effect on damaged brain tissue. It has been observed in animal models that women have a decreased susceptibility to traumatic brain injury and this protective effect has been hypothesized to be caused by increased circulating levels of estrogen and progesterone in women. A number of studies Studies in animals have confirmed that progesterone has a neuroprotective effect when administered soon after traumatic brain injury. Encouraging results have been reported in human clinical trials.
The mechanism for the protective effects of progesterone may be the reduction of inflammation that follows brain trauma.
Contenido relacionado
Human embryology
Eat (medicine)
Goniothalamus