Positron emission tomography
Positron emission tomography or PET (for the acronym in English of Positron Emission Tomography), is a health technology characteristic of a medical specialty called nuclear medicine.
PET is a technique similar to Computed Tomography (CT) in that the scanner detects radiation using a detector ring. However they differ in that the first technique uses radiation emitted from within the body while the second radiation is transmitted through the body.
Another fundamental difference with CT is that PET is a functional imaging technique. This means that it allows obtaining information about where and how a certain metabolic process is taking place within the organism. This is significantly different from the purpose of CT, which is a structural imaging technique, that is, it obtains information about the structure of tissues, not their function.
Positron emission tomography is an invasive technique —the radiopharmaceutical is injected intravenously— for diagnosis and investigation in vivo by imaging capable of measuring the metabolic activity of the human body. Like the rest of the diagnostic techniques in nuclear medicine such as SPECT, PET is based on detecting and analyzing the three-dimensional distribution that a radiopharmaceutical with an ultra-short half-life adopts inside the body, administered through an intravenous injection. Depending on what you want to study, different radiopharmaceuticals are used.
There are several medically useful positron-emitting radiopharmaceuticals. The most important of these is Fluorine-18, which is capable of binding to 2-deoxy-D-glucose to obtain the tracer Fluorodeoxyglucose (18FDG). Thanks to which, we will have the possibility of being able to identify, locate and quantify, through the SUV (Standardized Uptake Value), glucose consumption. This is a vitally important weapon in medical diagnosis, since it shows which areas of the body have high glucose metabolism, which is a fundamental characteristic of neoplastic tissues.
In addition to oncology, where PET has been widely implemented as a diagnostic technique, displacing CT as the first diagnostic option in some indications, other areas that benefit from this type of examination are neurology and cardiology. It also has a great role in clinical experimental studies.
History
In the late 1950s, David E. Kuhl, Luke Chapman, and Roy Edwards were the first to introduce the concept of emission and transmission tomography. His work led to the design and construction of several tomographic instruments at the University of Pennsylvania. In 1975, tomographic imaging techniques were developed by Michel Ter-Pogossian, Michael E. Phelps, Edward J. Hoffman, and others at the Washington University School of Medicine. The work of Gordon Brownell, Charles Burnham, and their associates at Massachusetts General Hospital contributed significantly to the development of PET technology, and the first demonstration of annihilation radiation for medical imaging was developed.
In 1961, James Robertson and his associates at Brookhaven National Laboratory built the first single-plane PET scanner, nicknamed the "head reducer. [] One of the most important factors for imaging was the development of radiopharmaceuticals. In particular, the development of labeled 2-fluorodeoxy-D-glucose (2FDG) by the Brookhaven group under the direction of Al Wolf and Joanna Fowler was an important factor in expanding the scope of PET imaging. The compound was first administered to two normal human volunteers by Abass Alavi in August 1976 at the University of Pennsylvania. Images of the brain obtained with an ordinary nuclear scanner (without PET) demonstrated the concentration of FDG in that organ. Later, the substance was used in dedicated positron tomographic scanners, to obtain the modern procedure. The logical extension of positron instrumentation was a design using two two-dimensional arrays. PC-I was the first instrument using this concept and was designed in 1968, completed in 1969, and reported in 1972. The first applications of PC-I in tomographic mode, as opposed to computed tomographic mode, were reported in 1970.
At the beginning of the 21st century, PET is an essential tool in the field of diagnostic imaging, with multiple clinical applications. Its use is very frequent both in Europe and in the United States, extending to the rest of the continents. The only limit is the price of the studies.
Today, modern Positron Emission Tomography equipment performs whole body studies in less than 20 minutes. In addition, a theoretical resolution of less than 0.5 cm has been achieved. These equipments are made up of multiple rings of detectors. A scanner is added to some of the PET equipment, and they become hybrid PET-CT equipment. In this way, the imaging technique is improved. These hybrid equipment also show a great advantage over PET-only equipment, since they allow the exact anatomical position of the focus of high metabolic activity to be indicated, and the rate of false negatives or positives is reduced. Small lesions can be targetedly identified.
Physical Fundamentals
PET imaging is based on the detection of radiation emitted by a Radioisotope injected into the patient. These radioisotopes are isotopes of a chemical element with an unstable nuclear configuration that emits radiation when it decays to a stable form in a process known as radioactive decay.
The radioactivity of the isotope depends on the stability of the nucleus based on the relationship between its atomic and mass number. In general, for elements with an atomic number less than 20, a 1:1 ratio is necessary for the configuration to be stable.
Radioactive Decay
A radioactive decay is the emission of particles from an unstable nucleus, which loses energy. The ultimate objective of disintegration is due to trying to find a more stable form, based on modifying the ratio of protons and neutrons in the atomic nucleus. To achieve this goal, radiation will be emitted.
Decay is a process that uniquely characterizes each radioisotope. In the case of PET, radiopharmaceuticals are sought whose effective half-life is short, since by emitting ionizing radiation (high energy) it is necessary to seek the least impact on the patient's body.
Radiation emission can be mainly of three types: α particle emission, β particle emission or γ radiation.
α particle emission
An α particle is a 4He nucleus, that is two protons and two neutrons. The emission of an α particle follows the reaction:
^{A-4}_{Z-2}Y + ^{4}_{2}He^2+}}}" xmlns="http://www.w3.org/1998/Math/MathML">XZAΔ Δ AndZ− − 2A− − 4+He2+24{displaystyle {ce {^{A}_{Z}X- PHP ^{A-4}_{Z-2}Y + ^{4}_{2}He^2+}}}}} ^{A-4}_{Z-2}Y + ^{4}_{2}He^2+}}}" aria-hidden="true" class="mwe-math-fallback-image-inline" src="https://wikimedia.org/api/rest_v1/media/math/render/svg/56e647e4d31f4df885c0fd12fffb79c14183c785" style="vertical-align: -1.171ex; width:22.557ex; height:3.509ex;"/>
This radiation is not interesting for the PET technique
Emission of β particles
A β particle is either an electron or a positron, giving rise to two types of radiation, β- and β+ respectively. The reactions corresponding to β- and β+ radiations are, respectively:
p^{+}{}+e^{-}{}+{bar {nu _{e}}}}}}" xmlns="http://www.w3.org/1998/Math/MathML">nΔ Δ p++e− − +.. e! ! {displaystyle {ce {n-negativep^{+}{}{}{}{{-}{cH00FF00}}}}p^{+}{}+e^{-}{}+{bar {nu _{e}}}}}}" aria-hidden="true" class="mwe-math-fallback-image-inline" src="https://wikimedia.org/api/rest_v1/media/math/render/svg/14fb2f4d5d5a11ad7d0be67f4a0768cee96acbb6" style="vertical-align: -0.671ex; width:19.552ex; height:2.843ex;"/>
An unstable atomic nucleus with an excess of neutrons can undergo a β- decay where a neutron becomes a proton, an electron, and an electron antineutrino (the antiparticle of the neutrino).
n{}+e^{+}{}+{nu _{e}}}}}" xmlns="http://www.w3.org/1998/Math/MathML">p+Δ Δ n+e++.. e{displaystyle {ce {p^{+}-purn{}+e^{+}{+{nu _{e}}}}}}n{}+e^{+}{}+{nu _{e}}}}}" aria-hidden="true" class="mwe-math-fallback-image-inline" src="https://wikimedia.org/api/rest_v1/media/math/render/svg/7d13fe09176a5eef5ae3370792e4bf501a5067e1" style="vertical-align: -0.671ex; width:19.552ex; height:2.843ex;"/>
unstable atomic nuclei with an excess of protons can undergo β+ decay, also called positron decay, where a proton becomes a neutron, a positron, and an electron neutrino.
A β particle is practically equivalent to an electron or a positron, the difference between these particles is the nuclear origin of the β particles.
In the case of PET, it is interesting to inject radionuclides that emit β+ radiation into the patient
Gam radiation emission
It corresponds to electromagnetic radiation (photons) with energies of the order of MeV or frequencies higher than 1019Hz. It is not a disintegration itself, it is rather a decay to lower energy levels. The nuclear configuration is maintained, there is only an energetic reduction.
There is no radioisotope that decays directly by emitting gamma radiation. This radiation is associated with the emission of very energetic photons from metastable intermediate species, not from the radioisotope directly. It is a radiation associated with a beta type radiation that has been produced previously.
^{A}_{Z}X + gamma}}}" xmlns="http://www.w3.org/1998/Math/MathML">XmZAΔ Δ XZA+γ γ {displaystyle {ce {^{A}_{Z}X^{m}-negative ^{A}_{Z}X + gamma}}}}}} ^{A}_{Z}X + gamma}}}" aria-hidden="true" class="mwe-math-fallback-image-inline" src="https://wikimedia.org/api/rest_v1/media/math/render/svg/53252edbfc4e503f5e1119134993bc6bae88de3d" style="vertical-align: -0.838ex; width:17.216ex; height:3.176ex;"/>
Electron Capture
Alternative process to positive beta decay for low emission energies. An inner electron is captured by the nucleus. A proton from the nucleus binds to this electron, forming a neutron. Due to the hole it has left, outermost electrons "fall" in a cascade, emitting characteristic radiation.
This phenomenon of radiation emission is not really interesting for the PET technique but for X-rays
Image formation
As the β+-emitting radioisotope injected into the patient decays, it emits positrons. Each of these can collide with a cortical electron from the tissue in which the radiopharmaceutical is present. This annihilation essentially gives rise to the emission of two 511keV gamma rays in the same direction and in opposite directions:
gamma + gamma}}}" xmlns="http://www.w3.org/1998/Math/MathML">e++e− − Δ Δ γ γ +γ γ {displaystyle {ce {e^+ + e^- - 2005 gamma + gamma}}} gamma + gamma}}}" aria-hidden="true" class="mwe-math-fallback-image-inline" src="https://wikimedia.org/api/rest_v1/media/math/render/svg/a82079400c1bcec01b19f8c5b169dbc941c0072c" style="vertical-align: -0.838ex; width:18.388ex; height:3.009ex;"/>
The image is obtained thanks to the fact that the CT scanners are capable of detecting these gamma photons emitted by the patient. In order for these photons to end up forming the image, they must be detected "in coincidence", that is, at the same time; in a suitable time window (nanoseconds), and they must also come from the same direction and opposite directions. In addition, its energy must exceed a minimum threshold that certifies that it has not suffered significant energy dispersions on its way (scatter phenomenon) to the detectors. This uptake makes it possible to deduce that the radioisotope is on the line that joins the diametrically opposite detectors. This line that joins both detectors is called the response line (LOR). The coincidence window is directly dependent on the ability of the detector crystal to produce light. Thanks to the axial symmetry of the detectors, data storage in the PET equipment is simplified. Each acquisition is recorded based on its polar coordinates (r, θ) and this representation is called a sinogram. In addition, at the end of the acquisition, the number of annihilations in each direction has been recorded, which makes it possible to assign different intensities to the final image depending on the concentration of the radiopharmaceutical. These sinograms are similar to projections captured by a CT scanner. However, the number of events recorded during the acquisition is much lower in the case of PET, so the images appear noisier.
In practice, it is necessary to carry out a pre-processing of the data to try to reduce or correct random coincidences, photons that have suffered scatter and other factors that introduce noise. On the other hand, for the reconstruction of the image itself, the use of Filtered Back Projection (FBP) is common due to its reduced computational cost. It is possible to use other algorithms for the reconstruction that take into account the statistics of the collected data, for example, the Shepp-Vardi algorithm.
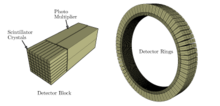
Scanner
The PET machine is very similar to the one used to do a CT scan. It is a large ring-shaped machine. Inside, the patient is placed on a stretcher. Before starting the test, a radiopharmaceutical must be administered to the patient. It can be intravenously, orally or inhaled, depending on the diagnostic suspicion. The PET scanner must be designed to detect coincidences in the emission of gamma rays by the radiotracer. The detection system consists of a set of detection rings made up of independent modules called detector blocks. Each detector block is a matrix structure of scintillation crystals coupled to a number of photomultiplier tubes whose function is to transform electromagnetic energy into electrical impulses. The most commonly used scintillation crystal is bismuth germanate (BGO). This solution of independent modules is very efficient since each detector block has its own electronics, therefore, while one block detects an event and is therefore unable to record another within that time window, the rest of the blocks can continue recording independently.
PET Properties
Speed
It is not a fast technique, so the patient's movement is a limitation and therefore a problem for this technique. Making it not a technique with a good resolution.
A PET scan can last anywhere from 30 minutes to 3 hours. After this time, the radioisotope has decayed to a very low level, eg the half-life of FDG is 108 minutes.
Ionizing radiation
Gamma rays, like X-rays, are high-energy radiation and therefore dangerous. It is an ionizing radiation that can be absorbed by tissues and interact with it. It must be controlled and not be excessive as it can cause burns and mutations.
PET scanner requires CT scanner
PET measures concentrations of radioisotopes through the gamma rays that are emitted. It must be taken into account that gamma rays are attenuated by the tissues they pass through. Not all tissues absorb the same amount of radiation, therefore, in order not to falsify the concentration measurements, it is necessary to obtain the attenuation map to correct the PET readings.
Medical applications
Oncology
The use of 18FDG by oncological processes is based on the fact that a fundamentally anaerobic metabolism occurs inside tumor cells, which increases the expression of glucose transporter molecules (from GLUT-1 to GLUT-9), increased hexokinase isoenzyme, and decreased glucose-6-phosphotase. The 18FDG is captured by the cells but since it cannot be metabolized, it suffers a "metabolic trap" thanks to which the images are obtained.
Thus, the PET allows us to estimate the foci of abnormal cell growth throughout the organism, in a single study, since it is a study of the whole body, therefore it will allow us to know the extension. But it also serves, among other things, to evaluate the response to treatment in control studies, by comparing the behavior of metabolism in the areas of interest between the two studies.
For the patient, the examination is neither uncomfortable nor painful. It should be consulted in the case of lactating or pregnant women since in these situations the test should be delayed, or not performed. You should go fasting for 4-6 hours, avoiding physical exercise on the day before the examination and without withdrawing the usual medication. Hyperglycemia may make it impossible to obtain adequate images, making it necessary to repeat the study later. After the injection of the radiopharmaceutical, the patient will remain in a rest room. The exploration lasts approximately 30-45 minutes.
Cardiology
The most common application of the PET technique in the field of cardiology is the study of myocardial viability, using 18F-FDG as a radiotracer. Myocardial viability is defined as the existence of myocardial tissue altered in terms of contractility and perfusion but that is capable of recovering function if coronary flow is restored. This is an important study to be able to differentiate patients with coronary disease or ventricular dysfunction who may benefit from myocardial revascularization techniques instead of undergoing heart transplantation.
By means of PET we can distinguish a hibernating Myocardium (potentially reversible) from a stunned Myocardium. The myocardium uses fatty acids as its primary source of energy, the metabolism of which requires an important oxidative process. However, when this oxygen supply decreases, the myocardium changes its metabolism towards anaerobic glycolysis. Therefore FDG uptake is preserved or increased.
It is also necessary to study myocardial perfusion through the use of ammonium labeled with nitrogen-13.
Neurology
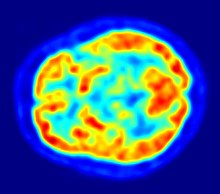
The PET technique also allows the study of neurodegenerative diseases such as Alzheimer's disease, other dementias or Parkinson's, through the metabolic study of the brain.
FDG is used as a radiotracer since brain metabolism is based on glucose metabolism. PET makes it possible to distinguish Alzheimer's disease with high reliability due to the observation of a decrease in glucose metabolism. Defined patterns of metabolic alteration can also be observed in the case of parkinsonism and the study of this hypometabolism in patients with epilepsy makes it possible to differentiate which patients could benefit from surgery.
In addition, using PET it is possible to diagnose cerebrovascular diseases by studying cerebral vascular perfusion. For this diagnosis it is necessary to use oxygen-15 as a radiopharmaceutical
Patient preparation
For the patient, the test is neither painful nor uncomfortable. They must wear metal-free and comfortable clothing.
It is important that the patient come fasting; do not eat or drink anything except plain (non-carbonated) water for at least 4 hours before the start of the test. He must drink a lot of water to ensure that he comes to the exam hydrated.
If the patient is diabetic, special care must be taken. This is because FDG is very similar to glucose, the balance between blood sugar and insulin levels can have a large impact on the quality of PET images and therefore greatly influence the ability to detect tumors on images. This can lead to a complex process, since both high blood sugar and high insulin can produce very poor quality images and lead to misinterpretation of the results. The goal is to plan your food intake and medication doses so that your insulin levels are fairly low, but your blood sugar is not too high. This is usually accomplished by fasting and not taking your medications in the moments leading up to your PET/CT scan. Therefore, the diabetic patient must schedule the insulin intake in such a way that it does not need to be administered 4 hours before the test. Before the test begins, a glucose measurement will be taken. It must be less than 180 to be tested.
Should be avoided during pregnancy, especially in the first trimester, as there is a risk of radiation to the fetus. It is also advisable to avoid this type of test during lactation since some radiopharmaceuticals can be eliminated in breast milk, so it is advisable to inform the doctor that you are breast-feeding before performing the test. As a solution, mothers should avoid breastfeeding after performing the test. In anticipation of the period of time in which she will not be able to breastfeed, the mother can express milk before the test and store enough to cover the child's needs during that period. The time to wait after the test will depend on the radiopharmaceutical administered, but in general it is a few hours.
In order to accurately interpret your CT scan, we need to know a number of details about your health and past medical history. Before the test, the patient should inform the technician of the following:
- Drugs you're taking.
- Surgery and other major medical procedures to which it has been subjected, including the dates of each.
- Information about chemotherapy treatments you have received, including the date of your last therapy.
- Information about radiation therapy treatments you have received, including dates and part of the treated body.
- Any other type of cancer treatment you have received.
- Any bone marrow stimulant medication and the date it last took it.
- All recent diagnostic imaging studies (CT, PET/CT, MRI, etc.) that have made it
Most patients will need to drink several cups of oral contrast before the scan or else it will be injected. After administering the radiopharmaceutical, the patient must remain at rest. The approximate duration of the test can vary from 30 minutes to 2 hours.
Contenido relacionado
Differential mechanism
Brig
Ravinder N. Maini