Parkinson's disease
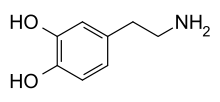
Parkinson's disease (PD), also called Parkinson's disease, idiopathic parkinsonism, shaking palsy or simply Parkinson's, is a chronic neurodegenerative disease characterized by bradykinesia (slow movement), rigidity (increased muscle tone), tremor, and loss of postural control. This disease is due to a deficit in the secretion of dopamine, a hormone released by the nerve endings of the substantia nigra.
Parkinson's disease is often classified as a movement disorder; however, it also triggers changes in cognitive function, depression, pain, and changes in the function of the autonomic nervous system.
This disease represents the second most common neurodegenerative disorder, behind Alzheimer's disease. It is widespread throughout the world and affects both males and females, affecting between 1% to 2% of the population over 60 years of age or 0.5% to 5% of the population over 65 years of age. The disease can present from the age of 40 and its incidence increases with age, especially in men.
Parkinson's disease increases in severity over time, as a consequence of the progressive destruction, for reasons that are still unknown, of the pigmented neurons of the substantia nigra.
In 1997, the World Health Organization established that World Parkinson's Day would be celebrated on April 11, with the aim of raising awareness of the needs of people suffering from this ailment. This date was established because it corresponds to the birth of James Parkinson, the British doctor who first described "shaking palsy", a term he himself coined.
Classification
Parkinson's disease is classified into clinical stages according to the degree of involvement of the patient.
But you always have to keep in mind that each person is affected differently:
There are several rating scales that can be used as tools to determine disease progression. Criteria for evaluating Parkinson's disease focus on the severity of motor disturbances and the degree of impairment in a person's daily activities.
Generally used rating scales, such as the Hoehn and Yahr scales, focus on motor disturbances. These alterations are evaluated according to their severity on a scale from 1 to 5. On this scale, depending on the difficulties a person has in carrying out their activities, a score of 1 and 2 (mild to moderate) is assigned in the early stage of the condition., score of 2 and 3 (moderate to severe) in the middle stage and a score of 4 and 5 (severe to disabling) in the most advanced stage of the disease.
The Parkinson's Disease Rating Scale (UPDRS) is more comprehensive than the Hoehn and Yahr scales. It takes into account the disturbance in carrying out daily activities, behavior, mood, cognitive complications, and the effects of treatment regarding motor disturbances.
History
In 1817, James Parkinson, an English physician, described a syndrome he called Paralysis Agitans, which was later named Parkinson's disease by Jean-Martin Charcot in 1861.
Epidemiology
Globally, the annual incidence of Parkinson's disease is eighteen new cases per hundred thousand inhabitants, but the high life expectancy that patients usually have means that the prevalence of the disease in the population is quantitatively higher than the incidence, registering about one hundred and sixty-four cases per hundred thousand inhabitants. According to studies sponsored by the Europarkinson study group, the prevalence of Parkinson's disease in the European continent is 1.43% in people over sixty years of age, although estimates have been made in states such as Spain or United Kingdom, which state that close to one hundred and twenty thousand inhabitants are affected by this disease in both countries. In North America, the figure shoots up to one million patients suffering from this disease, with 1% of the population over 65 years of age being affected.
However, this incidence is increasing over time since it is estimated that in the year 2040 the number of people suffering from Parkinson's will have doubled, reaching approximately 14 million patients. This is why we talk about the Parkinson's Pandemic.
In early ages, specifically before the age of forty, Parkinson's disease is exceptional and its prevalence is less than 1/100,000. The incidence of this disease begins to increase from the age of fifty and does not stabilize until the eighties, although this fact may be the result of a selection bias.
Several studies have revealed a marked prevalence of Parkinson's disease in rural areas, especially among men. This may be because life in the countryside sometimes includes different risky environmental exposures, such as contamination in well water from the use of pesticides and insecticides.
Mortality
Studies on mortality in Parkinson's disease are limited by the inaccuracy of death certificates, as well as diagnostic confusion between idiopathic Parkinson's and other types of neurodegenerative disorders. With all this, it can be established that mortality rates are low for any age stratum and that the age of death of patients has been shifting to more advanced ages, due to a progressive increase in life expectancy. In addition, everything seems to indicate that treatment with levodopa reduces the risk of death in patients, especially during the first years of the disease. In fact, and indeed, the standardized mortality of Parkinson's disease stood at 2.9 before the introduction of levodopa, since after the appearance of the drug the figure underwent a colossal decrease that left it at 1.3, providing patients with a life expectancy that was close to normal. However, a systematic review of the effect of levodopa on change in life expectancy showed that the improvement that had occurred as a result of drug treatment was less, with a standardized mortality estimate of 2.1.
When death occurs in patients suffering from Parkinson's disease, it is usually due to an intercurrent infection, generally thoracic, or trauma produced in one of the falls caused by postural instability. It should be noted that patients with Parkinson's disease have a lower probability of dying from cancer or cardiovascular diseases than the general population. [citation required]
Etiology
The exact cause of Parkinson's disease is currently unknown, but everything seems to indicate that it is a combination of certain environmental factors, genetics, oxidative damage and the normal aging process, with a probable pivotal role for the gut-brain connection. Parkinsonism has been documented to be associated with undiagnosed celiac disease and improvement with gluten removal from the diet. Neurological symptoms may be the only manifestation of gluten sensitivity, in the absence of digestive or other symptoms.
Although epidemiological studies show that one of the most prevalent risk factors is family history, toxic-environmental etiological theories have become increasingly important to the detriment of genetic theories.
Current evidence supports the hypothesis that Parkinson's disease begins in the gut and spreads through the sympathetic and parasympathetic nervous systems to the substantia nigra and central nervous system.
Studies conducted to date have found a higher risk of developing Parkinson's disease among personnel occupationally exposed to certain pesticides, mainly insecticides and herbicides. Other factors have been linked to an increased risk of developing Parkinson's disease, such as drinking pesticide-contaminated well water from farming and rural life, although it has not been possible to determine whether they are related to exposure to pesticides. pesticides or if they are independent risk factors.
Neurodegeneration
During maturation, a process occurs that involves the progressive degeneration and/or death of neurons. This process, which can be normal and natural during normal aging, involves the fundamental cells of the nervous tissue and its internal components, which are what prevent the effectiveness of conducting information in the human brain, with the consequent decrease in functions. cognitive. Thus, during normal aging, brain functions are limited in the affected area, but different neurological pathologies can also appear in humans, called neurodegenerative diseases. When neurons are lost in the brain, in the brainstem, which is Parkinson's disease occurs at the junction between the brain and the spinal cord, caused by the neurodegeneration of neurons crucial for the coordination of movement. This progressive neurodegeneration is what produces the characteristic motor symptoms of Parkinson's.
Pathogenesis
Parkinson's disease is characterized by the loss or degeneration of dopaminergic neurons in the substantia nigra and the formation of Lewy bodies in these neurons.
The alteration of alpha-synuclein and its accumulation in Lewy bodies has a greater extension and affects other areas and neuronal systems, such as the cholinergic, noradrenergic and serotonergic.
Clinical picture
Early symptoms are important to slow the progression of the disease as soon as possible - possibly many years before the onset of motor symptoms - due to indications of possible Parkinson's disease. These are:
- Years before the apparition, damage to the sense of smell
- Fluctuation of mood (light irritability) with light depressions
- Constipation
- The most typical, the disruption of paradoxical sleep through strong atypical movements during it (normally immobile healthy state) REM sleep (up to shouting or hitting)
Four motor symptoms are considered cardinal in Parkinson's disease: tremor, slowness of movement (bradykinesia), rigidity, and postural instability.
Rest tremor is present in about 85% of Parkinson's disease cases. The absence of facial expression, decreased blinking and movement of the arms when walking complete the clinical picture.
Many of these symptoms are common in the elderly and may be caused by other conditions. In patients with some of these parkinsonian symptoms, and with the absence of tremors, present in 15% of patients with Parkinson's disease, other pathologies of the nervous system, such as hydrocephalus, can be suspected. Specifically, normal pressure hydrocephalus also appears in the elderly, impairs the functions of the nervous system, leading to dementia, and presents with symptoms similar to those of Parkinson's, without the appearance of tremors. The diagnostic test to confirm or rule out normal pressure hydrocephalus is a CT.
Motor manifestations
- Bradicinesia.
- Alteration of fine motor.
- Micrograph (state in which the patient's handwriting is becoming smaller and more illegible).
- Hypotony.
- Sialorrea (overproduction of saliva).
- Sleep tremor from 4 to 6 Hz. Not rhythmic. Not regular.
- Muscle stiffness.
- Sign or dented wheel phenomenon.
- Alteration of posture.
- Postal inability.
Not all symptoms appear in all patients and the evolution and progression of the disease is highly variable depending on the case.
The type of tremor that appears in patients with Parkinson's disease consists of a kind of agitation that appears when the patient is at rest, but decreases when the patient is doing some activity or during sleep.
The condition may present with a slight twitch in which the tremor usually affects the arm, hand or fingers, known as a "pill-popping motion" or "coin-counting motion" characterized by a rolling motion forward and backward of the thumb and index finger. Tremor symptoms initially affect only one side of the body.
Loss of balance can cause the patient to fall and cause injury. This difficulty and the loss of the ability to maintain posture are mainly affected by walking, turning and standing. Also when trying to get up or leaning forward. That is why it is recommended to use a walker or a cane.
Bradykinesia or slow movements means that the patient has to work twice as hard to perform daily tasks because precision movements such as buttoning buttons or writing are especially affected. As the disease progresses, you may have difficulty getting up from your chair, turning over in bed, and have to walk slowly. A "freeze" usually occurs for a short time when you are walking.
Because it is a progressive disorder, symptoms gradually worsen over time. In general, the symptoms are aggravated by stress and emotional situations that cause anxiety. The psychological part is very important. Symptoms usually improve with rest, sleep, and relaxation techniques or any strategy to control stress and anxiety.
Non-motor manifestations
- Depression and anxiety.
- Apathy.
- Cognitive alterations.
- Sleep disorders.
- Sensory alterations and pain.
- Anosmia (loss or decrease in the sense of smell).
- Disorders of the autonomic function.
- Dementia.
Sometimes patients report leg pain from cramping, cold, burning, or numbness, and headache (cephalea) or lower back pain.
Difficulty sleeping is caused by anxiety, pain, or muscle stiffness. It is essential that the patient sleep well and get a good rest because restful sleep reduces the symptomatic effects of parkinsonism. Fatigue is a state of physical and mental exhaustion very common in parkinsonian patients. It may be the result of medications, depression, or the extra effort needed to perform daily tasks and cope with the symptoms of the disease. This can be improved with the appropriate medication if the cause that causes it is identified.
Depression can be caused by illness or a reaction to it. Some patients become depressed when they are diagnosed. Signs of depression include disturbances in sleep, memory, appetite, interest in social or sexual life, loss of energy or motivation for certain things, and a negative self-concept. The patient finds it difficult to accept her condition and becomes angry at her limitations.
Anxiety appears in any stressful situation, from not being able to perform daily tasks as the patient was used to or from having to speak in public. Anxiety can even lead to increased instability, shortness of breath, and excessive sweating. To prevent this from happening, relaxation techniques are very helpful.
Among the cognitive alterations, there are usually difficulties in concentration, memory, slowed thinking, the ability to plan complex tasks or to perform several tasks at the same time. When the degree of deterioration of cognitive functions is very advanced, Parkinson's Disease Dementia (PDD) occurs.
The emotional support of the people who surround the patient is fundamental and a key component in the care of the Parkinsonian because it provides numerous benefits.
The confusion and hallucinations that may occur are side effects of the parkinsonian medication and not of the disease itself.
Autonomic dysfunction is accompanied by various manifestations: orthostatic hypotension, constipation, micturition urgency, excessive sweating, seborrhea. Orthostatic hypotension can be caused by both sympathetic denervation of the heart and a side effect of dopaminomimetic therapy.
Depression affects approximately 50% of patients with Parkinson's disease and can occur at any time during the course of the disease, however it must be taken into account that it can be aggravated by the administration of antiparkinsonian and psychotropic agents; Other causes of depression refractory to treatment include: hypothyroidism, hypogonadism, vitamin B12 deficiency.
Psychotic symptoms (rather than a genuine psychosis it is the semiology of dementia) affect 6-45% of patients, in early stages they include visual hallucinations, although depression and dementia are the main triggers of the psychosis, so is the administration of dopaminergic agents, anticholinergics, amantadine, selegiline.
Diagnosis
The diagnosis of Parkinson's disease is based on the clinic, since no biological marker of this disease has been identified. For this reason, its diagnosis is based on the detection of the characteristic rigidity-tremor-bradykinesia triad and the absence of atypical symptoms, although it is also important to exclude other possible disorders by means of brain imaging techniques or laboratory tests. sanguine.
Diagnosis can be very complex. This difficulty in diagnosis is common to appear in the early stages of the disease, when the symptoms that the patient presents can be attributed to other disorders. A direct consequence of this fact is the elaboration of erroneous diagnoses.
It is important within the semiology of Parkinson's disease, to carry out an exhaustive questioning to find out other possible causes that differentiate Parkinson's disease with other possible extrapyramidal syndromes, since at the beginning there is no clear difference in the diagnosis by clinical features that are shared by other movement disorders.
There is no laboratory test or radiological study that allows the diagnosis of the disease, although some genetic diagnostic companies do offer tests for the sequencing of the SPARK1, SPARK2 and SPARK4 genes highly related to the disease, although the detection of mutations in these genes does not strictly determine the future development of the disease in the individual. This type of test is aimed at families with a high incidence of Parkinson's disease and the vast majority of patients present a specific mutation in one of these SPARK genes. In these cases, the gene in which the family mutation occurs could be sequenced in one of their descendants, although even so, the existence or not of the mutation does not ensure the presence of the disease. With all this, it is not even advisable to carry out this type of sequencing if no symptoms of the disease have previously appeared. Being a serious disease and currently without a cure, patients rarely prefer not to know their future with respect to Parkinson's.
It is also frequent that blood tests are carried out in order to rule out other possible disorders, such as hypothyroidism, liver dysfunction or autoimmune pathologies. On the other hand, brain imaging techniques, such as magnetic resonance imaging, positron emission tomography or single photon emission tomography, are effective in excluding other diseases that trigger symptoms similar to those of the disease of Parkinson's, such as a stroke or brain tumor.
It is common for physicians to ask the patient questions in order to determine if the patient consumed some kind of narcotic or if they were exposed to viruses or environmental toxins, in order to determine if a specific factor could have been the cause of parkinsonism. The patient's muscle activity is observed for a period of time, as specific motor disorders become more evident as the disease progresses.
A diagnostic indication is usually the therapeutic test, which consists of the application of pharmacological therapy with levodopa (which is considered the drug of choice in the treatment of Parkinson's disease) for at least 30 days closely observing the evolution of the patient. A positive test is considered if it radically responds to levodopa treatment and it is considered negative if there is no response at all. The therapeutic trial with levodopa is usually confirmatory if the disease is suspected; However, if the test is negative, the doctor will have to continue investigating other probable causes of the disorder or carry out more in-depth studies such as genetic markers.
Genetic markers of dementia in Parkinson's disease
Parkinson's Disease dementia (PDD) is the highest degree of cognitive deterioration and there are a series of genetic mutations that determine a greater predisposition of the patient to develop it; that is, a Parkinson's patient who possesses this genetic mark is more likely to suffer from PDD than a non-carrier patient. The RIMS2 gene locus variant rs182987047 is a confirmed mutation, and the TMEM108 gene locus variants rs1382073281 and the WWOX gene locus rs8050111 are potential candidates.
Epigenetic markers for diagnosis in Parkinson's disease
As well as genetic markers, epigenetic modifications related to this pathology have been identified. Three differentially methylated positions have been detected in blood samples from PD patients. Two of them were close to the SLC7A11 and FKBP5 genes. Previously, it has been described that the FKBP5 gene increases its expression progressively with age and this increase correlates with Braak staging in human brains and tau pathology. However, to determine the predictive ability of these markers, more in-depth clinical phenotyping and the use of larger cohorts are necessary.
Treatment
The treatment of Parkinson's disease consists of improving, or at least maintaining or prolonging the functionality of the patient for as long as possible. At present, the treatment can be of three types: pharmacological, surgical and rehabilitative.
Pharmacological treatment
Many of the characteristic symptoms of Parkinson's disease are due to a deficiency of dopamine in the brain, but the supply of this neurotransmitter to the patient with the aim of replenishing depleted stores is not effective, since dopamine cannot pass from the bloodstream to the brain. For this reason, the drugs that are used in the treatment of Parkinson's disease (anti-Parkinsonian drugs) use other pathways to temporarily restore dopamine in the aforementioned organ, or they mimic its actions.
Despite initial optimism, none of the drugs used to treat Parkinson's disease act on the progression of the disease. Currently, the most widely used drugs are levodopa and various dopamine agonists, although others such as selegiline (MAO-B inhibitor), amantadine (dopamine releaser) or benztropine (muscarinic receptor antagonist) also have some relevance. acetylcholine).
Levodopa
Levodopa, an oral drug that is combined with carbidopa or benserazide, thus achieving a reduction in the necessary doses and a damping of peripheral side effects. The structure of levodopa allows it to enter the brain, where it is converted into dopamine. Around 80% of patients treated with levodopa show an initial improvement, especially in terms of rigidity and hypokinesia, while 20% of people fully recover motor function.
Dopaminergic agonists
The effectiveness of dopamine agonists on symptom control, especially on bradykinesia and rigidity, is significantly less than that of levodopa, but this is partly offset by a longer half-life and shorter incidence of development of "on-off" phenomenon and dyskinesias. With the exception of cabergoline, the rest can be used in monotherapy or associated with levodopa. These drugs are being used more and more as sole treatment in the early stages of Parkinson's disease, as long as there is no predominance of tremor, in order to delay the introduction of levodopa as long as possible.
Bromocriptine, a derivative of the alkaloids of Claviceps purpurea, is a potent dopamine agonist in the central nervous system. An inhibitor of the adenohypophysis, it was initially used to treat conditions such as galactorrhea or gynecomastia, but its efficacy was later confirmed in Parkinson's disease. Its action lasts longer than levodopa, so it is not necessary to administer it as frequently. Bromocriptine was expected to be effective in those patients who ceased to respond to levodopa due to loss of dopaminergic neurons, but this fact has not yet been confirmed. Among its adverse effects, nausea and vomiting stand out, but others such as nasal congestion, headache, blurred vision or arrhythmias can also occur.
Other dopamine agonists are lisuride, whose adverse effects are similar to those of bromocriptine, its administration is parenteral and it is currently not approved for the treatment of Parkinson's disease in the US, only in Europe; pergolide, which is the most potent and one of those with the longest half-life, however this medication was withdrawn from the US market in March 2007 due to its association with heart valve disease; pramipexole, a non-ergoline compound that has important clinical effects on tremor and depression; ropirinol, which, like the previous one, is a non-ergoline compound, but unlike it, it can cause sleep crises; and cabergoline, which is an ergoline derivative, with a long elimination half-life that allows once-daily administration. It should be noted that the last three dopamine receptor agonists are the most recently introduced into the pharmacological landscape.
Monoamine oxidase B inhibitors: selegiline
Selegiline is a selective MAO inhibitor for MAO-B, which is predominant in dopamine-containing areas of the central nervous system. With the inhibition of MAO-B, it is possible to protect dopamine from intraneuronal degradation, so this drug was initially used as a complement to levodopa.
After discovering the role of MAO-B in neurotoxicity, the possibility was raised that selegiline could have a neuroprotective effect, delaying the progression of the disease.
Presynaptic dopamine releasers: amantadine
The accidental discovery in 1969 that amantadine was beneficial in Parkinson's disease caused it to stop being used solely as an antiviral drug, which was what it had been designed for. Although scientists do not know exactly how it works, numerous possible mechanisms of action have been proposed based on neurochemical evidence indicating that it increases dopamine release, inhibits amine reuptake, or acts directly on dopamine receptors. With all this, recent studies have brought to light that it inhibits the action of glutamate, a brain chemical that causes the generation of free radicals.
In addition to not being as effective as levodopa or bromocriptine, the action of amantidine is diminished over time. In contrast to this, its side effects are qualitatively similar to those of levodopa, but ostensibly less important.
Currently, amantadine associated with levodopa is used to achieve control of motor disorders, especially dyskinesia, and to prolong the useful life of levodopa.
Transcranial stimulation
Transcranial alternating current stimulation or TACS
Cancels the brain signal that causes tremors by applying a small electrical current, through electrodes on the outside of a patient's head. So it does not carry the risks associated with deep brain stimulation. TACS works by placing two electrode pads on the patient, one near the base of the neck and one on the head, above the motor cortex (the part of the brain involved in tremor control). The alternating current applied by the electrodes is made to coincide with the oscillating tremor signal, so as to cancel it out, and the physical tremor is suppressed. The preliminary study has been carried out with 15 people with Parkinson's disease at the John Radcliffe Hospital in Oxford. The researchers demonstrated a 50% reduction in resting tremors among the patients.
Transcranial magnetic stimulation
Transcranial or transcranial magnetic stimulation is a technique based on stimulating the brain using magnetic pulses generated by a device. Evidence shows that it improves upper extremity function in the short term, and gait and general motor symptoms of Parkinson's disease in the short and long term. However, more research is needed to develop optimal therapeutic protocols. for the application of this technique.
Surgical treatment
In the mid-20th century, neurosurgery was the most common method used to treat the tremor and rigidity characteristic of patients with Parkinson's disease, but the problem was that it was not always successful. in surgical interventions and in the serious complications that used to arise. With this panorama, the use of surgery was reduced from 1967 with the introduction on the market of levodopa, an alternative treatment that provided more safety and efficacy. But with the technological progress experienced in recent years, new brain imaging techniques have been achieved that have allowed surgical precision to be improved, neurosurgery recovering its popularity as a treatment for some people with Parkinson's disease who, for various reasons, no longer respond to drug treatment.
Studies in recent decades have led to great improvements in surgical techniques, so surgery is once again being used in people with advanced Parkinson's disease for whom drug therapy is no longer sufficient.
Surgery for PD can be divided into two large groups: lesional brain stimulation and deep brain stimulation (DBS). The areas of action of the ECP or lesions include the thalamus, the globus pallidus or the subthalamic nucleus.
Deep brain stimulation (DBS) is the most widely used surgical treatment, developed in the 1980s by Alim-Louis Benabid and others. It involves the implantation of a medical device called a brain pacemaker, which sends electrical impulses to specific parts of the brain. DBS is recommended for people who have Parkinson's disease with motor fluctuations and tremor not controlled by medication, or for those who are intolerant of medication, as long as they do not have severe neuropsychiatric problems.
Another, less common surgical treatment is the intentional induction of lesions to suppress hyperactivity in specific subcortical areas. For example, pallidotomy involves surgical destruction of the globus pallidus to control dyskinesia.
Nerve transplantation
In 1982, Parkinson's disease became the first neurodegenerative condition for which brain tissue transplantation was performed, with the goal of promoting dopamine production in affected areas of the brain.
Rehabilitation treatment
It is important that patients exercise their hands, but more important is that a speech therapist works with the patient for as long as possible, since they must correct dysphagia, handling objects, hypophonia, anxiety, micrographs, and others aspects of language that only this professional can do.
If with the pharmacological treatment it is possible for patients to improve in terms of motor symptoms, the same does not happen with balance, since it worsens throughout the course of the disease. In fact, several studies have been carried out that demonstrated that no changes in global balance are experienced in patients with Parkinson's disease in relation to the administration of drug treatment.[citation needed]
Prevention
Multiple studies have been carried out in order to identify exogenous factors that could modify the risk of developing Parkinson's disease. Through retrospective case-control studies, attempts have been made to associate the regular consumption of non-steroidal anti-inflammatory drugs and certain vitamins with a lower risk of contracting the disease, but the results obtained are contradictory and it is not possible to infer that the consumption of these drugs reduces the risk. The strongest association at this time is the higher incidence of Parkinson's disease among non-smokers: there is a relationship between the alteration of dopamine levels produced by smoking and a decreased risk of contracting Parkinson's, but the mechanisms of that relationship have not yet been determined.
In various studies carried out recently in which the relationship of Parkinson's disease with tobacco was not only investigated, but also with coffee, it was confirmed that the consumption of both reduces the risk of suffering from this disease because a A series of receptors and substances, such as the dopamine mentioned above, could protect neurons related to this condition. However, more studies are needed on this topic to verify this theory. In addition, the author of a publication maintains that thinking that smoking is good is self-deception and inconsistency. For example, there is a myth based on studies that the incidence of Parkinson's disease decreases in smokers when the reality is that the fact that fewer smokers have Parkinson's disease is largely due to the fact that people who smokers live less, and the incidence of Parkinson's disease increases in later life (when smokers have usually died of cancer or cardiovascular disease).
Some studies suggest a relationship between dairy consumption and Parkinson's disease.
Research
Research on Parkinson's disease has advanced and there is a better understanding of the disease. This is facilitating the development of more accurate tools for diagnosis, which currently continues to be based on clinical signs, and new treatments, although levodopa remains the most effective treatment to date.
In May and June 2016, several major discoveries were made in the United States. On the one hand, researchers from Northwestern University in Chicago discovered a new cause of Parkinson's disease related to mutations in a gene called TMEM230. Days later, researchers at the University of Pittsburgh School of Medicine in the United States discovered why the Parkinson's-related alpha-synuclein protein —a major constituent of Lewy bodies that are the pathological hallmark of Parkinson's disease— Parkinson's—is toxic to neurons in the brain.
Parkinson's disease has genetic relationships with numerous human traits and characteristics, which may help in understanding the pathology. For example, in a study published in the journal Nature in 2016, a positive genetic correlation was observed with intracranial volume.
Neuroprotective treatments
Neuroprotection research is at the forefront of PD research. Many molecules have been proposed as potential treatments. However, none have been conclusively shown to reduce degeneration. Agents currently under investigation include anti-apoptotics (omigapil, CEP-1347), antiglutamatergics, monoamine inhibitors oxidase (selegiline, rasagiline), promitochondrial (coenzyme Q10, creatine), calcium channel blockers (isradipine), and growth factor (GDNF). Preclinical research also points to alpha-synuclein. Two vaccines preparing the human immune system to destroy alpha-synuclein, PD01A and PD03A, (developed by the Austrian company Affiris), have completed phase I human clinical trials.
Contenido relacionado
Lymphocyte
Anabolic steroid
Neuroanatomy