Obesity
Obesity is a chronic disease characterized by the excessive accumulation of adipose tissue in the body, that is, when the natural energy reserve of humans and other mammals — stored as body fat—increases to a point where it threatens health or life. Obesity is the fifth leading risk factor for human death in the world. Every year, at least 2.8 million adults die as a result of obesity.
The World Health Organization (WHO) defines obesity as when the body mass index (BMI, the ratio of an individual's weight to height squared) is equal to or greater than 30 kg/m². An abdominal circumference greater than or equal to 102 cm in men and greater than or equal to 88 cm in women is considered a sign of obesity (see Diagnosis of obesity).
Obesity is part of the metabolic syndrome and is a known risk factor, that is, it indicates predisposition to several diseases, particularly cardiovascular diseases, type 2 diabetes mellitus, sleep apnea, stroke and osteoarthritis, as well as some forms of cancer, dermatological and gastrointestinal conditions. (See Effect on health).
Although obesity is an individual clinical condition, it has become a serious and growing public health problem:
Obesity has reached epidemic proportions worldwide. [...] Although it was previously considered a problem confined to high-income countries, obesity is now also prevalent in low- and middle-income countries.Article of the World Health Organization
Classification
According to its causes, obesity is classified into the following types:
- Exogenous obesity: obesity due to an inadequate diet, in conjunction with a low physical activity.
- Endogenous obesity: the one that causes metabolic alterations. Within endogenous causes, endocrine obesity is spoken when it is caused by dysfunction of some endocrine gland, such as thyroid (hypothyroid obesity) or sexual hormone deficiency, such as gonadal obesity.[chuckles]required]
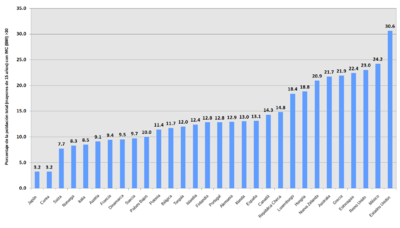
Childhood overweight and obesity
Increase in childhood overweight and obesity
Childhood obesity is one of the most serious public health problems of the 21st century. The problem is global and is progressively affecting many low- and middle-income countries, especially in urban areas. The prevalence has increased at an alarming rate. The number of children and adolescents affected by obesity has increased more than 10 times, from 11,000,000 (eleven million) in 1975 to 124,000,000 (one hundred and twenty-four million) in 2016.
Obese and overweight children tend to remain obese into adulthood and are more likely to develop noncommunicable diseases such as diabetes and cardiovascular disease at earlier ages. Overweight, obesity and related diseases can, to a large extent, be prevented. Therefore, high priority must be given to the prevention of childhood obesity.[citation needed]
Epidemiology
Each year, at least 2.8 million adults die from the health consequences of being overweight or obese. They are also responsible for between 7% and 41% of certain types of cancer, 23% of ischemic heart disease cases and 44% of diabetes cases, which currently affects 347 million people worldwide. the world.
In the UK, the Health Survey predicted that more than 12,000,000 (twelve million) adults and 1,000,000 (one million) children would be obese by 2010 if no action was taken.
In the United States, obesity is a public health problem due to its prevalence, costs, and burden on health services and government agencies, as well as private medicine have warned for years about adverse effects for health associated with overweight and obesity. Despite warnings, the problem is getting worse, and in the United States, the prevalence of overweight and obesity makes obesity a major public health problem. In 2004, the CDC reported that 66.3% of adults in the United States were overweight or obese. The cause in most cases is the sedentary lifestyle; approximately 40% of adults in the United States do not participate in any physical activity during their leisure time and less than a third of adults engage in the recommended amount of physical activity. The United States has the highest rate of obesity in the developed world. From 1980 to 2002, obesity has doubled in adults, and the prevalence of overweight has become critical in children and adolescents. Statistics show a rapid growth of the obesity epidemic in the United States between 1985 and 2004 and of 2003 to 2004, "of children and adolescents ages 2-19, 17.1% were overweight...and 32.2% of adults 20 and older were obese". This sudden increase in the prevalence of obesity is attributed to environmental and population factors rather than individual and biological behavior due to the rapid and continuous increase in the number of overweight and obese individuals.
In China, median income increased due to the economic boom. People in China have recently started a more sedentary lifestyle and at the same time started consuming more high-calorie foods. From 1991 to 2004, the percentage of adults who were overweight or obese increased from 12.9 to 27.3%.
In Mexico, according to the 2012 National Health and Nutrition Survey (ENSANUT2012), overweight and obesity affect seven out of 10 Mexican adults. The combined prevalence of overweight or obesity is 73% for women and 69.4% for men of adulthood. School-age children (both sexes), ages 5 to 11, had a combined national prevalence of overweight and obesity in 2012 of 34.4%, 19.8% for overweight and 14.6% for obesity. 35% of adolescents between the ages of 12 and 19 are overweight or obese. One in 5 adolescents is overweight and one in ten is obese. The combined national prevalence of overweight and obesity in adolescents was around 35.8% for females and 34.1% for males. In children under five years of age, it has increased between 1988 and 2012, going from 7.8 to 9.7%, respectively. The main increase in the combined prevalence of overweight and obesity is observed in the northern region of the country, with 12%. Mexico City had 39.9% overweight and 33.9% obesity, and the southern zone of Mexico presented 39.6% overweight and 31.6% obesity. The northern region of the country had a prevalence of overweight of 35.9% and obesity of 37.2%.
Etiology
The causes of obesity are multiple, and include factors such as genetic inheritance; the behavior of the nervous, endocrine and metabolic systems, and the lifestyle of each person. For Mazza (2001), 30% of obesity cases can be attributed to genetic factors, 40% to non-heritable factors, and 30% to merely social factors; that is, 70% of cases can be attributed to environmental factors. The mechanisms by which these factors contribute to excess body fat are:
- a calorie intake greater than the body needs, and
- a physical activity less than the body needs.
If more energy is ingested than necessary, it accumulates as fat. If more energy is consumed than is available, fat is used for energy. Therefore, obesity is produced by excess energy, as a result of alterations in the energy input/output balance. As a consequence, various complications can occur, such as arterial hypertension, diabetes mellitus and coronary diseases.
Inheritance plays an important role. So much so that for a person who comes from an obese couple, the risk of becoming obese is 10 times higher than normal. In part, this is due to metabolic tendencies of fat accumulation, but also, in part, because cultural eating and sedentary habits contribute to repeating patterns of obesity from one generation to the next.[citation required ]
Another percentage of those who suffer from obesity is attributed to hormonal or endocrine diseases, which can be solved through specialized diagnosis and treatment.[citation needed]
Lifestyle
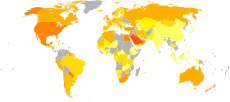
1600 kcal per capita per day1600-1800 kcal per capita per day1800-2000 kcal per capita per day2000-2200 kcal per capita per day2200-2400 kcal per capita per day
2400-2600 kcal per capita per dayMost research has concluded that the combination of excessive nutrient intake and sedentary lifestyle are the main factors contributing to the rapid acceleration of obesity in Western society in the last quarter of the century XX.
Despite the wide availability of nutrition information in schools, doctors' offices, the Internet, and grocery stores, it is clear that overconsumption of food continues to be a substantial problem. For example, confidence in energy-dense fast food has tripled between 1977 and 1995, and calorie consumption has quadrupled in the same period.
However, food consumption by itself is insufficient to explain the phenomenal increase in obesity levels in the industrialized world in recent years. An increase in sedentary lifestyle also plays a significant role in the current elevated levels of this disease.
Less established lifestyle issues that may influence obesity include mental stress and insufficient sleep.
Heredity and genetics
As with many medical conditions, the caloric imbalance that results in obesity often develops from a combination of genetic and environmental factors. Polymorphisms in several genes that control appetite, metabolism, and adipokine integration predispose to obesity, but the condition requires the availability of sufficient calories and possibly other factors to fully develop. Several genetic conditions that have obesity as a trait have been identified (such as Prader-Willi syndrome, Bardet-Biedl syndrome, MOMO syndrome, leptin and melanocortin receptor mutations), but single locus mutations have only been reported. been found in 5% of obese individuals. Although it is thought that a large proportion of the causative genes remain unidentified, for the most part obesity is probably the result of interactions between multiple genes where non-genetic factors are also likely to be important.
A 2007 study identified several common mutations in the FTO gene; heterozygotes had a 30% higher risk of obesity, while homozygotes had a 70% increased risk. Thanks to another GWAS study, conducted in 2015, it has been possible to identify more than 100 genetic variants involved in modulating BMI and waist/hip ratio. These parameters provide information on body weight and fat distribution, aspects closely related to obesity and its pathophysiological effects. Likewise, knowledge of these polymorphisms provides information on the biological mechanisms that underlie the relationship between age/sex and body size/shape, facilitating diagnosis and favoring a much more personalized treatment of obesity. On the other hand, it identifies genetic loci (locuses) that contribute to the differences that exist in sexual dimorphism between males and females.
At the population level, the thrifty gene hypothesis, which postulates that certain ethnic groups may be more prone to obesity than others, and the ability to take advantage of rare periods of abundance and use this abundance to store energy efficiently may have been an advantage. evolutionary, in times when food was scarce. People with higher fat reserves were more likely to survive the famine. This tendency to store fat is probably a maladjustment in a society with a stable food supply.
Diseases
Approximately 2% to 3% of the causes of obesity are endocrine diseases such as hypothyroidism, Cushing's syndrome, hypogonadism, hypothalamic lesions or growth hormone deficiency.
Untreated celiac disease and non-celiac gluten sensitivity, which often present without digestive symptoms and in most cases remain undiagnosed, are a poorly understood cause of obesity in both children and adults. More than Half of adults are obese at the time of being diagnosed with celiac disease and only 15% are below their normal weight. These rates are somewhat lower in children. Recent evidence shows that in some cases the persistence of certain complications of celiac disease, which do not subside despite following a gluten-free diet, predisposes them to overweight and obesity. Among them are they include gallbladder disorders, exocrine pancreatic insufficiency, increased intestinal permeability, intestinal bacterial overgrowth, non-alcoholic fatty liver disease, lactose intolerance, and milk allergy.
Also certain mental illnesses can predispose to obesity or increase the risk of obesity such as eating disorders such as bulimia nervosa and binge eating or food addiction. Quitting smoking is a known factor in moderate weight gain, as nicotine suppresses appetite. Certain medical treatments (steroids, atypical antipsychotics, and some fertility drugs) can cause weight gain.
Apart from the fact that correcting these situations can improve obesity, the presence of an increase in body weight can complicate the management of other diseases.
Neurobiological Mechanisms
Flier summarizes the many possible pathophysiological mechanisms involved in the development and maintenance of obesity.
This field of research has been almost unattainable until the discovery of leptins in 1994, thanks to which many other hormonal mechanisms involved in the regulation of appetite and food consumption, as well as storage patterns in the brain, have been elucidated. adipose tissue and in the development of insulin resistance.[citation needed]
Since the discovery of leptins, other mediators have been studied such as ghrelins, orexins, PYY 3-36, cholecystokinin, adiponectin and adipokines, which are mediators produced by adipose tissue; its action is thought to be modified by many obesity-related diseases.[citation needed]
Leptins and ghrelins are considered complementary in their influence on appetite, ghrelins, produced by the stomach, modulate short-term appetite control (to eat when the stomach is empty and to stop when the stomach is full). Leptin is produced by adipose tissue to signal stored body fat stores and mediate long-term appetite control (eating more when fat stores are low and less when fat stores are high). Although leptin administration may be effective in a small group of obese subjects who are leptin deficient, many more obese individuals appear to be leptin resistant. This resistance partly explains why the administration of leptins has not been shown to be efficient in suppressing appetite in the majority of obese subjects.
While leptin and ghrelin are produced peripherally, their appetite control is through their actions on the central nervous system. In particular, these and other appetite-related hormones act on the hypothalamus, a brain region central to regulating food intake and energy expenditure. There are several loops within the hypothalamus that contribute to this appetite integration role, with the melanocortin pathway being the best understood.
The circuit begins in the arcuate nucleus of the hypothalamus, which has outputs to the lateral (HL) and ventromedial (VMH) hypothalamus, the feeding and satiety centers in the brain, respectively.
The arcuate nucleus contains two distinct groups of neurons. The first group coexpresses neuropeptide Y (NPY) and agouti related peptide (AgRP) and receives stimulatory signals from the lateral hypothalamus and inhibitory signals from the ventromedial hypothalamus. The second group coexpresses proopiomelanocortin (POMC) and cocaine-amphetamine-regulated transcripts (CART) and receives stimulatory signals from the ventromedial hypothalamus and inhibitory signals from the lateral hypothalamus.
Consequently, NPY/AgRP neurons stimulate eating and inhibit satiety, while POMC/CART neurons stimulate satiety and inhibit eating. Both groups of neurons in the arcuate nucleus are regulated in part by leptin. Leptin inhibits the NPY/AgRP group, while it stimulates the POMC/CART group. Thus a deficiency in leptin signaling, via leptin deficiency or leptin resistance, leads to overeating and may account for some forms of genetic and acquired obesity.
Microbiological aspects
The role of bacteria and archaea that colonize the digestive tract in the development of obesity has recently begun to be the subject of research. Bacteria are involved in digestion (especially of fatty acids and polysaccharides), and alterations in the 10-tape ratio may explain why certain people are more likely to gain weight than others.
In the human digestive tract, bacteria are generally members of the phylum Bacteroides or Firmicutes. In obese people, there is a relative abundance of firmicutes (which cause relatively high energy uptake), which is restored by weight loss. Whether this imbalance is the cause of obesity or an effect cannot yet be concluded from these results. Microorganisms speculated to be associated with obesity include the archaea Methanobrevibacter smithii.
Social determinants
Some obesity cofactors are resistant to the theory that the epidemic is a new phenomenon. In particular, a class cofactor that appears consistently across many studies. Comparing net worth with body mass index, a 2004 study found that in the United States, obese subjects are half as wealthy as thin ones.
When income differentials were compared, inequity persisted, lean subjects were hereditarily richer than obese subjects. A higher rate of a low level of education and tendencies to rely on cheap fast food is seen as a reason why these results are so different. Another study found that women who married into higher status were predictably thinner than women who married into lower status.
A 2007 study of 32,500 children in the original Framingham study cohort followed for 32 years indicated that BMI changes in friends, siblings, or spouses regardless of geographic distance. The association was strongest between mutual friends and lowest between siblings and spouses (although these differences were not statistically significant). The authors concluded from these results that acceptance of body mass plays an important role in changes in body size.
Regarding body mass indices (BMI) in rural locations, the most recent longitudinal analyzes of global trends in BMI, by area of residence (rural and urban), indicate that more than 80% of the increase in the average BMI in low- and middle-income regions is due to its increase in rural areas, which affects women more and is occurring at the same rate, or even faster, than in urban areas of these regions (NCD Risk Factor Collaboration, 2019).
Environmental factors
While it might often seem obvious why a certain individual gains weight, it is more difficult to understand why the average weight of a certain society has recently been increasing. While genetic causes are central to understanding obesity, they cannot fully explain why one culture gains more weight than another.
This is most noticeable in the United States. In the years just after World War II until the 1960s, the average weight per person increased, but few became obese. In the two and a half decades since the 1980s, the growth in the rate of obesity has accelerated markedly and it is increasingly becoming a public health problem.
There are a number of theories to explain the cause of this change since the 1980s. The most credible is a combination of several factors.
- Loss of activity: obese people are less active in general than thin people and not precisely because of their obesity. A controlled increase in calorie consumption of thin people does not make them less active, correspondingly when obese people lose weight do not start to be more active. Weight change does not affect activity levels.
- Lower relative cost of food: massive changes in agricultural policies in the United States and America have led to a decline in food prices at the consumer level, as at no time in history. The current debate on trade policies highlights disagreements on the impact of subsidies. In the United States, corn production, soy, wheat and rice is subsidized through the so-called US Farm Bill. Maize and soy, which are the main source of sugar and fat in processed foods, are therefore cheaper compared to fruits and vegetables.
- Increased marketing: this also played a role. At the beginning of the 1980s, the Reagan administration in the United States raised most of the regulations concerning propaganda for children on sweets and fast food. As a result, the number of propaganda seen by the average of children increased greatly and a long proportion of them consumed fast and sweet meals.
- The change in the workforce: every year a greater percentage of the population spends its full day of work behind a desk or computer, without doing virtually any exercise. The consumption of dense frozen foods in calories that are cooked in the microwave oven (very comfortable) has increased and the production of snacks increasingly elaborated.
- A social cause that many believe plays a role is the increase in the number of families with two incomes, in which none of the parents remains at home to take care of the house. This increases the number of restaurants and meals to take.
- Uncontrolled expansion of cities can be a factor: the obesity rate increases to the extent that the expansion of cities increases, possibly because there is less time to walk and cook.
- Since 1980 fast-food restaurants have seen dramatic growth in terms of the number of sales and consumers treated. Low-cost meals and intense competition for a portion of the market have led to an increase in the size of portions, such as portions of McDonald's fries, increased from 200 calories in 1960 to more than 600 calories today.
Menopause
Menopause produces changes in the distribution of body fat and in the oxidation of adipose tissue. The increase in abdominal and visceral fat mass of the postmenopause is accompanied by an increase in antioxidant capacity due to hormonal changes, while age has no influence. However, antioxidant capacity has a linear correlation with age, but not with truncal fat mass.
In initially premenopausal women who were followed for 4 years throughout the menopausal transition, age-associated increases in abdominal subcutaneous fat were reported, while menopause is accompanied by increases in total body fat mass and in visceral fat mass. The American SWAN study links the increase in visceral fat during menopause with changes in bioavailable testosterone.
Excess body weight (overweight and obesity) produces greater alterations in the Kupperman Index, metabolism, sleep and quality of life. Obese menopausal women also have a higher prevalence of problems with their sexuality, related to themselves and factors related to their partners.
Clinical picture
Effects on health and associated diseases
The WHO states that “Overweight and obesity are the fifth leading risk factor for death worldwide. Every year at least 2,800,000 (two million eight hundred thousand) adults die as a result of being overweight or obese. Furthermore, 44% of the burden of diabetes, 23% of the burden of ischemic heart disease, and between 7 and 41% of the burden of some cancers are attributable to overweight and obesity."
A large number of medical conditions have been associated with obesity and the health consequences are the result of increased body fat: (osteoarthritis, sleep apnea, diabetes, cancer, cardiovascular disease, non-alcoholic fatty liver disease).
Mortality is increased in obesity: with a BMI greater than 32, they are associated with a double risk of death.
There are alterations in the body's response to insulin with (insulin resistance), a pro-inflammatory state, and an increased tendency to thrombosis (pro-thrombotic state).
The association with other diseases may be dependent or independent of the distribution of adipose tissue. Central obesity (or obesity characterized by a high waist-to-hip ratio) is an important risk factor for metabolic syndrome, the cluster of a number of diseases and risk factors that strongly predispose to cardiovascular disease. These are type 2 diabetes mellitus, high blood pressure, high blood cholesterol and triglyceride levels (combined hyperlipidemia).
In addition to metabolic syndrome, obesity is also correlated with various other complications. But it has not yet been determined to what extent obesity is a direct cause of some of these ailments or if they have some other cause (for example, a sedentary lifestyle).[citation required]
- Cardiovascular: congestive heart failure, increased heart size and associated arrhythmias and dizziness, lung corps, varices and pulmonary embolism.
- Endocrine: polycystic ovary syndrome, menstrual disorders and infertility.
- Gastrointestinal: gastro-esophageal reflux disease, fatty liver, colelitiasis, hernia and colorectal cancer.
- Renal and génito-urinario: erectile dysfunction, urinary incontinence, chronic kidney failure, hypogonadism (men), breast cancer (women), uterine cancer (women),
- Obstetric: Acute fetal suffering with intrauterine fetal death.
- Teguments (piel and appendices): estrías, nigrican acantosis, lymphedema, cellulite, forums, intertrigo.
- Skeletal muscle: hyperuricemia (which predisposes to gout), loss of mobility, osteoarthritis, back pain.
- Neurological: stroke, paresthetic meralgia, headaches, carpal tunnel syndrome; cognitive impairment, dementia and depression; idiopathic intracranial hypertension.
- Respiratory: dyspnea, obstructive sleep apnea or Pickwick syndrome, and asthma.
- Psychological: depression, low self-esteem, dismorphic body disorder, social stigmatization.
While being severely obese has many health complications, those who are overweight also face a small increase in mortality or morbidity. On the other hand, some studies have found that osteoporosis occurs less in slightly obese people, suggesting that the accumulation of fat, especially visceral, which is measured by abdominal circumference, is a protective factor for bone mineralization.
Diagnosis
In a practical way, obesity can typically be diagnosed in terms of health by measuring body mass index (BMI), but also in terms of your fat distribution by waist circumference or waist/waist ratio measurement. hip. Furthermore, the presence of obesity needs to be considered in the context of other risk factors and associated comorbidities (other medical conditions that could influence the risk of complications).
BMI
Body mass index is a simple and widely used method of estimating the proportion of body fat. The BMI was developed by the Belgian statistician and anthropometrist Adolphe Quetelet. It is calculated by dividing the subject's weight (in kilograms) by the square of their height (in meters), therefore it is expressed in kg/m².
Government agencies in the United States determine overweight and obesity using the Body Mass Index (BMI), using weight and height to determine body fat. A BMI between 25 and 29.9 is considered overweight and any value over 30 is obese. Individuals with a BMI above 30 increase the risk of various health hazards.
The WHO (World Health Organization) establishes a commonly used definition with the following values, agreed in 1997, published in 2000 and adjusted in 2010:
- BMI less than 18.5 is below normal weight.
- IMC 18.5-24.9 is normal weight
- BMI of 25,0-29,9 is overweight.
- IMC 30.0-34.9 is class I obesity.
- BMI of 35,0-39,9 is class II obesity.
- BMI of 40,0 or greater is class III obesity, severe (or morbid).
- BMI of 35,0 or greater in the presence of at least one or another significant morbidity is also classified by some people as morbid obesity.
In a clinical setting, doctors take into account race, ethnicity, muscle mass, age, gender, and other factors that may affect the interpretation of BMI. BMI overestimates body fat in very muscular people, and on the other hand body fat can be underestimated in people who have lost muscle and bone mass (many elderly). Mild obesity, as defined by BMI, is not a cardiovascular risk factor and therefore BMI cannot be used as a sole clinical and epidemiological predictor of cardiovascular health.
Waist circumference
BMI does not take into account the differences between adipose tissue and lean tissue; nor does it distinguish between different forms of adiposity, some of which may be more closely associated with cardiovascular risk.
The better understanding of the biology of adipose tissue has shown that central obesity (male-type or apple-type obesity) has a greater relationship with cardiovascular disease than BMI alone.
Absolute waist circumference (>102 cm in men and >88 cm in women) or waist-hip ratio (>0.9 for men and >0.85 for women) are used as measures of central obesity.
In a cohort of nearly 15,000 subjects from the National Health and Nutrition Examination Survey (NHANES) III study, waist circumferences explained significantly better obesity-related health risk factors than BMI when metabolic syndrome was taken as a measure.
Body fat
An alternative way to determine obesity is to measure the percentage of body fat. Doctors and scientists generally agree that a man with more than 25% body fat and a woman with more than 30% body fat are obese.
However, it is difficult to measure body fat accurately. The most accepted method has been to weigh people underwater, but underwater weighing is a procedure limited to laboratories with special equipment. The simplest methods for measuring body fat are the skinfold method, in which a pinch of skin is accurately measured to determine the thickness of the subcutaneous fat layer; or bioelectrical impedance analysis, usually carried out by clinical specialists. Its routine use is discouraged. Other measurements of body fat include CT scan, MRI, and dual energy x-ray absorptiometry.
Risk factors and associated morbidities
The presence of risk factors and disease associated with obesity are also used to establish a clinical diagnosis. Coronary artery disease, type 2 diabetes, and sleep apnea are life-threatening risk factors that may indicate clinical treatment for obesity. Smoking, hypertension, age and family history are other risk factors that could indicate treatment.
Treatment
You need to properly treat the underlying diseases, if they exist. From here it depends on seeking balance, through lifestyle adjustments, which exceeds dietary recommendations.
The main cause of obesity and excess body fat in general is high blood sugar levels. The proof of this is that more than 85% of diabetics in the world are obese or overweight, and diabetes and obesity have spread like an epidemic in the last decades practically at the same time. This alone incontrovertibly demonstrates a favorable relationship between an individual's body fat levels and blood sugar levels.
Although blood sugar levels between 70 and 110 mg/dL are called "normal", this does not mean that they are "good" for the body's health. Levels above 85 mg/dL already pose a high risk of developing obesity and diabetes in the future. Therefore, the only logical treatment for obesity is to reduce those levels below 85 mg/dL.
It has long been believed that excess body fat in a human body is due to a "caloric surplus", and that the key to eliminating it is a "caloric deficit". However, nowadays it is known that caloric deficit diets generally do not work more than to lose muscle weight, and that they can even force the human body to cling even more to lipid reserves.
The main dietary treatment for obesity is to reduce body fat by avoiding high-glycemic foods (which spike blood sugar) at all costs, especially GM wheat, corn, rice, and fourthly, white sugar, as well as carbonated or cola drinks, whether sugary or dietetic. It should also be considered that there are a number of substances that reduce the body's metabolism and therefore tend to deregulate blood sugar levels, such as: aspartame (extremely harmful artificial sweetener), hydrogenated oils, fluoride, aluminum (found in transgenic soy), lactose (found in cow's milk) and even fructose (fruits with high amounts of fructose should not be consumed if you want to lose body fat, contrary to the general recommendation that fruit is "healthy" »).
Unfortunately, most people think that the treatment for overweight and obesity is simply "eating less" due to the widespread erroneous theory that the amount of body fat depends on the body's caloric balance, when in fact it does not. anything other than blood sugar levels. In order to reduce caloric intake, the population tends to buy "low-fat" foods and, consequently, high in refined carbohydrates. The theory that the most important thing to lose fat is the glycemic index of food is not so widespread, and therefore almost no one knows that a piece of bread raises blood sugar even more than the same amount of white sugar. Therefore, the massive consumption of wheat is one of the main causes of obesity worldwide, since almost no one is aware of how extremely dangerous it is to consume it daily at lunch and dinner.
Clinical protocols
In a clinical practice guideline from the American College of Physicians, the following five recommendations are made:
- People with a higher body mass index of 30 should receive dietary advice, exercise and other relevant behavior factors to be intervened and establish a realistic goal for weight loss.
- If this goal is not achieved, drug therapy should be offered. Patients need to be informed of the possibility of side effects of medicines and the absence of information about the long-term safety and effectiveness of them.
- Drug therapy may consist of sibutramine, orlistat, phentermine, dietarypropion, fluoxetin, and bupropion. For the most serious cases of obesity, stronger drugs such as amphetamines and methamphetamines can be used selectively. The inheritance is not enough to recommend sertraline, topiramate or zonisamide.
- In patients with BMI greater than 40 who fail to reach their goal in weight loss (with or without medication) and those who develop obesity-related complications, the reference to bariatric surgery may be indicated. Patients should be warned of potential complications.
- Those who require bariatric surgery should be referred to high-volume reference centers, as evidence suggests that surgeons who frequently perform these procedures, that is to say they have greater practice and experience in them, have fewer complications.
A clinical practice guideline by the US Preventive Services Task Force (USPSTF) concluded that the evidence is insufficient to make a recommendation for or against routine behavioral advice to promote a healthy diet in unselected patients in primary care settings, however this intensive advice about dietary behavior is recommended in those patients with hyperlipidemia and other known risk factors for cardiovascular and related chronic diseases. Counseling can be carried out by primary care clinicians or by referral to other specialists such as nutritionists or dietitians.
Exercise
Exercise requires energy (calories). Calories are stored in body fat. During prolonged aerobic exercise the body initially consumes its fat stores in order to provide energy (this is not correct according to current scientific knowledge). The largest muscles in the body are the leg muscles, and these naturally burn the most calories, making walking, running, and cycling among the most effective forms of exercise for reducing body fat.
A meta-analysis of randomized controlled trials by the International Cochrane Collaboration found that "exercise combined with diet results in greater weight loss than diet alone".
Diet
In general, the dietary treatment of obesity is based on reducing food intake. Several dietary approaches have been proposed, some of which have been compared in randomized controlled trials:
A study comparing the Atkins, Zone, Weight Watchers, and Ornish diets over 6 months found the following results:
- The four diets generated a modest but statistically significant weight loss over the course of 6 months.
- Although the Atkins diet generates the highest weight loss in the first 4 weeks, weight loss at the end of the study was independent of the type of diet followed."
- The higher dropout rate for groups performing Atkins and Ornish diets suggests that many individuals find that these diets are too difficult to follow.
A meta-analysis of randomized controlled trials concluded that "compared with treatment as usual, dietary advice produces modest weight loss that diminishes over time."
Low Carb vs Low Fat
Many studies have focused on diets that reduce calories via low-carb diets (the Atkins diet, the Zone diet) vs. low-fat diet (the LEARN diet, the Ornish diet). The Nurses' The Health Study, an observational cohort study, found that low-carbohydrate diets based on plant sources of lean protein are associated with less coronary artery disease.
A 2002 meta-analysis of randomized controlled trials by the International Cochrane Collaboration concluded that fat-restricted diets are no better than calorie-restricted diets in achieving fat loss. long-term weight loss in people who are overweight or obese.
A more recent meta-analysis, including controlled studies published after the Cochrane review, found that "low-carbohydrate diets, in which energy is not restricted, appear to be at least as effective as in low-fat energy-restricted diets in Indians and weight loss for up to one year. However, potentially favorable changes in triglyceride and HDL cholesterol levels must be weighed against potentially unfavorable changes in LDL cholesterol when low-carbohydrate diets are used to induce weight loss".
The Women's Health Initiative Randomized Controlled Dietary Modification Trial study found that a diet with a total of 20% of the energy coming from energy and an increase in the consumption of vegetables and fruits up to at least 5 servings per day and grains up to at least 6 servings per day resulted in: no reduction in cardiovascular disease, no significant reduction in invasive breast cancer, and no reduction in colorectal cancer.
Additional recent randomized controlled studies have found that: A comparison of the Atkins, Zone, Ornish, and LEARN diets in premenopausal women found the greatest benefits from the Atkins diet.
For the choice of diet for a specific person, the measurement of individual insulin secretion can be taken into account. In young adults "reducing glycemic (carbohydrate) load may not be especially important in achieving weight loss among individuals with high insulin secretion". This is consistent with previous studies of diabetic patients in which low-carbohydrate diets carbohydrates were more beneficial.
Low glycemic index
“The glycemic index factor is a classification of carbohydrate-rich foods based on their overall effect on plasma glucose levels. Low-glycemic foods, such as lentils, provide a slower, more constant source of glucose into the bloodstream, thus stimulating less insulin release than high-glycemic foods, such as white bread."
Glycemic load is "the mathematical product of the glycemic index and the amount of carbohydrates."
A randomized controlled study, which compared four diets that varied in the amount of carbohydrates and the glycemic index, found complicated results:
- Diet 1 and 2 were high in carbohydrates (5% of total energy consumption).
- Diet 1 was high Glycemic Index
- Diet 2 was low Glycemic Index
- Diet 3 and 4 were high in protein (25 % of total energy consumption).
- Diet 3 was high Glycemic Index
- Diet 4 was low Glycemic Index
In diets 2 and 3 they lost the most weight and fat mass; however, low-density lipoproteins fell in diet two and increased in diet three. Therefore the authors concluded that low glycemic index high carbohydrate diets were the most favourable.
A meta-analysis conducted by the Cochrane Collaboration concluded that low glycemic index diets or low loads and indicated lead to more weight loss and better lipid profile. However, the low glycemic index and low load and clinical diets were pooled together and no attempt was made to separate the effect of load versus index.
Medications
Pharmacological treatment of obesity has an adjuvant role and is normally justified in patients with a BMI equal to or greater than 30 kg/m² or in patients with risk factors (diabetes or dyslipidemia) with a BMI equal to or greater than 27 kg/m².
Generally, the drugs used are divided into three large groups:
- anorexic drugs: noradrenergic, serotonergic or mixed action drugs (sibutramine, fluoxetin),
- drugs or substances that: inhibit the absorption of nutrients or fats (orlistat, chitosan) and
- a third heterogeneous group: composed of carbohydrate metabolism modulators (chromium typicine, ginseng), caloric spending stimulators (cafeine, ephedra alkaloids), fat synthesis reducers by increased oxidation (L-carnitine, hydroxycytric acid) and stimulators of saciedad (plántago, glucomana).
The most commonly prescribed medication for exercise/diet resistant obesity is orlistat (Xenical, which reduces intestinal fat output by inhibiting pancreatic lipase) and sibutramine (reductil, Meridia, an appetite suppressant anorectic). Weight loss with these drugs is modest, and in the long term the average weight loss with orlistat is 2.9 kg, with sibutramine 4.2 kg, and with rimonabant 4.7 kg. Orlistat and rimonabant lead to a reduction in the incidence of diabetes, and all drugs have some effect on lipoproteins (different forms of cholesterol).
However, there is little information about the long-term complications of obesity, such as heart attacks. All drugs have potential side effects and contraindications. Commonly weight loss drugs are used for a set period and are discontinued or switched to another agent if the expected benefit is not obtained, such as less than 5 weight loss. % of total body weight in a 12-week period for orlistat.
A meta-analysis of randomized controlled trials conducted by the International Cochrane Collaboration concluded that in diabetic patients fluoxetine, orlistat, and sibutramine, could achieve significant but modest weight loss between 12-57 weeks, with benefits in the long term on health not very clear.
Obesity may also influence the choice of drugs to treat diabetes. Metformin can lead to mild weight reduction (as opposed to sulfonylureas and insulin) and has been shown to reduce the risk of cardiovascular disease in obese type 2 diabetics. Thiazolidinediones, may cause slight weight gain, but they decrease "pathological" abdominal fat and can therefore be used in diabetics with central obesity.
Bariatric Surgery
Bariatric surgery (or “weight loss surgery”) is the set of surgical interventions used in the treatment of morbid obesity, that is, it is normally indicated for patients with a BMI equal to or greater than 40 kg/ m² or in patients with risk factors or comorbid associations with a BMI equal to or greater than 35 kg/m². As with any surgical intervention, complications can occur and bariatric surgery is frequent, so it should be considered as the last resort when dietary modification and pharmacological treatment have not been successful. The result of bariatric surgery depends on several mechanisms, the most common proposal is the reduction of stomach volume (for example with an adjustable gastric tape), thus producing a feeling of early satiety and reduced intake, while other procedures (such as gastric bypass) also reduce the length of the digestive tract that food comes into contact with, directly reducing absorption. The surgery in which the tape or band is used is reversible while the operations in which the stomach or intestine are shortened are not. Some procedures can be performed laparoscopically.
Two large studies have shown a mortality/benefit relationship from bariatric surgery with a marked decrease in the risk of diabetes mellitus, cardiovascular disease, and cancer. Weight loss was greatest in the first few months after surgery. surgery, but the benefit was maintained in the long term. In one of the studies there was an unexplained increase in deaths from accidents and suicides that did not outweigh the benefit in terms of disease prevention. Gastric bypass surgery was approximately twice as effective as the adjustable gastric band procedure.
Forecast
A study of people over forty years of age by the Framingham Heart Study from 1948 to 1990 revealed that non-smokers in overweight patients (BMI of 24 to 29.9 kg/m²) had a lower than average life expectancy of 3.3 years for women and 3.1 years for men. In obese patients (BMI greater than 30 kg/m²) non-smokers obtained 7.1 years less in women and 5.8 years less in men. Obese smoking patients had a lower life expectancy than the mean of non-obese smokers of 7.2 years for women and 6.7 years for men and compared to the mean of non-smokers of normal weight. it was a difference of 13.3 years for women and 13.7 for men.
Prophylaxis
Obesity can be prevented and treated by seeking a balance in caloric intake with a balanced diet taking into account the caloric intake of food. It is known that each 250 grams of fat is equivalent to 2,250 kilocalories, and each gram of fat is equivalent to 9 kcal. If there is excess body fat, the energy (measured in calories) they represent should be calculated and decreased in dietary intake for an appropriate period.
One method is based on estimating the energy contribution of the diet (metabolization energy) from its macronutrient content (and ethanol, in the case of including alcoholic beverages). This energy of metabolism is calculated from the Atwater factors, which are only valid for the diet and not for particular foods. These factors are listed in the following table:
| Nutrient/compound | Energy (kcal/g) |
|---|---|
| Grasa | 9.0 |
| Alcohol | 7.0 |
| Protein | 4.0 |
| Carbohydrate | 4.0 |
Thus, a daily diet that provides a total of 100.6 g of protein, 93.0 g of fat and 215.5 g of carbohydrates, will provide energy of approximately 2101 kcal.
As for food, the following table lists some Atwater factors that allow estimating the energy they would provide after metabolizing them:
| Food | Protein (kcal/g) | Grasa (kcal/g) | Carbohydrate (kcal/g) |
|---|---|---|---|
| egg | 4.36 | 9,02 | 3.68 |
| meat / fish | 4.27 | 9,02 | ♪ |
| milk / dairy | 4.27 | 8,79 | 3,87 |
| fruit | 3,36 | 8,37 | 3.60 |
| rice | 3,82 | 8,37 | 4,122 |
| soy | 3,47 | 8,37 | 4.07 |
You can also find out the energy that food would provide through a device called a «bomb calorimeter». With this system, the energy values that are usually included in most food composition tables are calculated. The following table reflects some examples:
| Output | Energy (kcal) |
|---|---|
| Full milk (a glass) | 156. |
| Whole yogurt (124 g) | 69 |
| Apple (a medium piece) | 77 |
| Teacup with two teaspoons of sugar | 67 |
Cultural and social significance
Etymology
The word "obese" comes from the Latin obēsus, which means 'stout, fat, or chubby'. Ēsus is the past participle of edere (‘to eat’), with the prefix ob added to it. In classical Latin, this verb is found only in the past participle form.
History
In numerous human cultures, obesity was associated with physical attractiveness, strength, and fertility, especially female fertility. Some of the earliest known cultural artifacts, such as Venus figurines, are pocket-sized figurines depicting an obese female figure. Although its cultural significance is unrecorded, its widespread use throughout prehistoric Mediterranean and European cultures suggests a central role for the obese female form, and its use in magical rituals suggests cultural approval of (and perhaps reverence for) this bodily form. This is most likely due to her ability to easily deal with children and survive famines.
Obesity was considered a symbol of wealth and high social status in post-Neolithic cultures prone to food shortages or famines. This was viewed in the same way until the early modern period in European cultures, but when food security for the majority of the population was achieved, it served more as a visible display of "lust for life", gluttony and immersion in the realm of the erotic. This was especially the case in the visual arts, such as the paintings of Rubens (1577-1640), whose regular depiction of overweight women gave rise to the descriptive term "Rubensian" fatness.
Obesity can also be seen as a symbol within a prestige system. «The type of food, the quantity and the way in which it is served are among the important criteria of social class. In most tribal societies, even those with a highly stratified social system, everyone - royalty and commoners - ate the same kind of food and if there was a famine everyone would be hungry. With the ever-increasing diversity of foods available, food has become not only a matter of social status, but also a mark of individual personality and taste."
Contemporary culture
In modern Western cultures, the obese body shape is widely considered unattractive and many negative stereotypes are commonly associated with obese people. Obese children, adolescents, and adults can also face heavy social stigma. Obese children are frequently the target of threats and are frequently rejected by their peers. Although obesity rates have increased since the turn of the 20th century among all social classes in the Western world, obesity is frequently seen as a sign of low socioeconomic status: the ancient poor were hungry and skinny, the modern poor eat the cheapest junk food, which makes them fat.
Most people have experienced negative thoughts about their body image, and some take drastic measures to try to change their shape, including diet, medication, or surgery. Not all contemporary cultures disapprove of obesity. There are cultures which are traditionally more condoning (to varying degrees) of obesity, including some African, Arab, Indian, and Pacific Islander cultures. Especially in recent decades, obesity has begun to be viewed more as a medical condition in modern Western culture, even referring to it as an epidemic.
A small but growing fat acceptance movement has recently emerged that seeks to challenge discrimination based on weight. Obesity support and acceptance groups have started a lawsuit to defend the rights of obese people and to prevent their social exclusion. Authors within this movement argue that the social stigma around obesity is founded on cultural anxiety and that public concern about the health risks associated with obesity are inappropriately used as a rationalization for this stigma.
Pop Culture
Various stereotypes of obese people have found their way into expression in popular culture. A common stereotype is the character of the obese person, who has a warm and dependable personality, however the stereotype of the vicious and obese bully (such as Dudley Dursley from the Harry Potter book series, Nelson Muntz from The Simpsons) is equally common.). Gluttony and obesity are commonly portrayed together in works of fiction. In cartoons, obesity is often used for comedic effect, with fat cartoon characters (such as Piggy, Porky Pig, and Tummi Gummi) having to squeeze through tight spaces, often getting stuck or even exploding.
A more unusual example of obesity-related humor is Bustopher Jones, from the poem by T. S. Eliot. Bustopher Jones: The Cat About Town featured in his book Old Possum's Book of Practical Cats, as well as the musical Cats, who became famous for being a regular visitor to many gentlemen's clubs. Due to his constant club lunches, he is extraordinarily overweight, being described by others as "a 25-pound...and he's gaining weight every day." Another popular character is Garfield, a cartoon cat, he is also obese for humor. When his owner, John, put him on a diet, instead of losing weight, Garfield slowed down his weight gain.
It is arguable that this representation in popular culture adds to and maintains commonly perceived stereotypes, damaging the self-esteem of obese people. On the other hand, obesity is often associated with positive characteristics such as humor (the stereotype of the jolly fat man like Santa Claus) and some people are more sexually attracted to obese people than thin people.
Non-medical consequences
In addition to the increase in disease and mortality there are other implications for the current global trend of obesity. Among these are:
- An increase in pressure on airline revenues (or increase in rates) due to pressure exerted to increase the width of seats in commercial aircraft and due to the higher cost of fuel: in 2000, the additional weight of obese passengers cost airlines and consumers 275 000 (two hundred and seventy-five million) of US dollars.
- An increase in litigation by obese people demanding restaurants (for causing obesity) and airlines (over the width of seats). The 2005 Food Consumption Personal Responsibility Decree was motivated by a need to reduce the number of litigation from obese activists.
- A considerable social and economic cost is attributable to obesity, with medical costs attributable to obesity increasing to 78,500,000 (sixty-eight billion) dollars or 9.1 percent of all medical expenses in the United States for 1988.
- A decrease in the productivity of workers measured by the use of permits for disability and absenteeism at work.
- A study by examining Duke University employees found that those with a higher BMI of 40 filled claim tables, twice more than the workers whose BMI was between 18.5 and 24.9 and lost working days more than 12 times more than other workers. The most common injuries were due to falls, affecting the lower limbs, hands, wrists and back.
Public health policies and measures
Public health and policy responses to obesity seek to understand and correct the environmental factors responsible for changes in the prevalence of overweight and obesity in a population. Neighborhood and being overweight are currently first and foremost political problems in the United States. Public health and policy solutions seek to change the environmental actors that promote calorie-dense, nutrient-poor food consumption and inhibit physical activity.
In the United States, policy has focused primarily on the control of childhood obesity, which has the most serious long-term public health implications. Efforts have been directed at key schools. Efforts are underway to reform the Federal meal reimbursement program, limit food marketing to children, and prohibit or limit access to sugar-sweetened beverages. In Europe, policy has focused on limiting marketing to children. There has been an international focus on the policy related to sugar and the role of agricultural policies in the production of foods that cause overweight and obesity in the population. To confront physical activity, efforts have been directed at examining zoning and access to parks and safe routes in cities.
In the UK, a 2004 report by the Royal College of Physicians, the School of Public Health and the Royal College of Paediatrics and Child Health entitled "Storing up problems", followed by a report by the House Health Committee of Commons, on the obesity act on health and society in the United Kingdom and possible approaches to the problem. In 2006, the National Institute for Health and Clinical Excellence (National Institute for Health and Clinical Excellence), published guidance on the diagnosis and management of obesity as well as the policy implications for non-care organizations such as councils. A 2007 report produced by Sir Derek Wanless for the King's Foundation warned that unless actions Additional measures are taken, obesity has the potential to cripple the NHS financially.
Contenido relacionado
Pneumotachograph
Sagittal plane
Rage