Measles
Measles is an infectious rash disease like rubella or chickenpox, quite common, especially in children, caused by a virus, specifically from the family paramyxoviridae of the genus Morbillivirus. As a pandemic disease it killed more than 200 million people. Among displaced people, the death toll from measles can be as high as 30%.
It is characterized by the typical red spots on the skin (rash), as well as fever and a general weakened condition. The cough is always present due to inflammation of the mucous membranes of the upper respiratory tract and responding to a classic of Infectious Diseases: "there is no measles without a cough". If complications develop, measles can cause life-threatening inflammation in the lungs and brain.
The incubation period for measles is usually 4 to 12 days, during which there are no symptoms. Infected people remain contagious from the onset of the first symptoms until 3 to 5 days after the rash appears.
The diagnosis is made through the clinical picture and the detection of antibodies in the blood. There is no specific therapy for the treatment of the disease; however, it can be prevented by administration of the measles vaccine. In the past, the MMR vaccine (also known as MMR) has reduced the number of infections. In most countries, the disease is notifiable to social health authorities.
In 1998, the World Health Assembly set the goal of eliminating endemic measles in Europe by 2007, in order to certify its elimination by 2010.
Cause
Humans are the sole host of the measles virus, a virus measuring around 120-140 nanometers with single-stranded RNA, a member of the paramyxovirus family (genus Morbillivirus). Two glycoproteins are found on the surface of the measles virus: the hemagglutinin or H protein and the fusion protein or F protein, forming a matrix of surface proteins. The H and F proteins are the proteins responsible for virus fusion with and inclusion within the host cell. The human cell receptors are CD150 or SLAM and to a lesser extent CD46. The vaccine produces antibodies in the individual directed against the surface proteins of the measles virus, in particular, against the H protein.
The WHO has reported 23 genotypes or genetic variants, grouped into eight serotypes (A-H). The mutation rate of the genomes is comparatively low, so the geographical areas of viral origin of the infection can be reconstructed with relative ease. In Central Europe, for example, genotypes C2, D6 and D7 have been located. Measles outbreaks in Switzerland and Bavaria in 2006/2007, on the other hand, were caused by the D5 genotype originating from Thailand or Cambodia. This allowed the detection of a chain infection, from Switzerland to Bavaria and from there to Austria and Hannover.. In addition, because in certain geographical regions there is only one stable serotype, the combination of elements coming from the surface of the pathogen allows the manufacture of a good vaccine for the region where it is found.
The virus is very sensitive to external factors such as high temperatures, ultraviolet radiation (light) and, due to its viral envelope, to many disinfectants such as those containing 1% sodium hypochlorite, 70% of ethanol, glutaraldehyde and formaldehyde. In the environment, it can be infectious for periods of up to two hours.
Pathogenesis
Transmission of the measles virus occurs by contact, coughing, or infected droplets from someone who is sick, who remains infectious three to five days before the rash appears until four days later. The virus penetrates the epithelial cells of the mucosa of the upper respiratory tract, such as the oropharynx or, less frequently, the conjunctiva of the eyes. The virus reaches the local lymphoid and reticuloendothelial tissue in less than 48 hours: tonsils, adenoids, thymus, spleen, etc., and the rest of the upper respiratory tract, where it reproduces, causing an initial asymptomatic viraemia during the first 4 days of infection. This is usually accompanied by a brief appearance of the virus in the blood. After about 5-7 days there is a second viremia, with consequent infection of the skin and respiratory tract. On the tenth day of infection, the host's immune response and interferon production begin, which progressively decrease viraemia, and the rash appears with the characteristic rash and other symptoms, such as cough and acute bronchitis, which define the rash period of the disease..
Through the invasion of the virus in the T-lymphocytes and an increase in the levels of messenger substances such as cytokines, in particular interleukin-4, a temporary immune weakness of the body is installed. During this phase, approximately four to six weeks, secondary infections may appear.[citation needed]
The body defends itself primarily with cellular immunity: cytotoxic T lymphocytes and natural killer cells. Patients with reduced immunity, based on a weakening of this part of the immune system, are at high risk of severe measles infection. However, it has been shown that a weakened immune system, which encompasses the area of the humoral rather than the cellular immune system, does not lead to an increased risk of disease. With the onset of rashes, antibodies appear, first of the IgM class and later of the IgG class.[citation needed]
Clinical picture
The incubation period is approximately 4-12 days (during which there are no symptoms). The first symptom is usually the appearance of high fever, for at least three days, cough, coryza (runny nose) and conjunctivitis (red eyes). Fever can reach 40°C (104°F). Koplik's spots that appear inside the mouth are pathognomonic (their appearance diagnoses the disease), but they are ephemeral: they disappear in about 24 hours.[citation needed]
Another symptom is a rash, which appears three to four days after the onset of fever. It is a reddish skin rash that disappears when pressed with a finger. The characteristic measles rash is described as a generalized, maculopapular rash that begins 2-3 days after the onset of fever and catarrhal symptoms. It first appears behind the ears, then spreads progressively to the forehead, cheeks, neck, chest, back, upper extremities, abdomen, and finally to the lower extremities, so it is said that the outbreak follows a head direction. feet, with slight itching. On the third day, the bud turns pale; on the fourth, it becomes brownish in color, it no longer rubs off with pressure and the skin tends to flake off; it disappears in the same order it appeared. For this reason, the rash is often said to 'spot', changing color from red to dark brown, before disappearing.
Cough is always present due to inflammation of the mucous membranes (mucositis) of the upper respiratory tract (nose, pharynx, larynx). From this appreciation arises an element of differential diagnosis with other rashes, responding to a classic of Infectious Diseases: "there is no measles without cough".
The rash and fever gradually subside over the seventh and tenth day, with the last traces of the rash usually disappearing by 14 days, with noticeable scaling.
Diagnosis and treatment
The clinical diagnosis of measles requires a history of fever for at least three consecutive days with at least one of the other three symptoms. Observation of Koplik's spots is also diagnostic of measles.[citation needed]
Alternatively, laboratory diagnosis of measles can be made by confirmation of IgM antibodies to measles, or isolation of measles virus RNA from respiratory specimens. In cases of measles infection after secondary vaccine failure, IgM antibodies may not be present. In such cases, serological confirmation can be established by detecting an increase in IgG antibodies by the ELISA immunoassay technique or complement fixation.[citation needed]
Contact with other patients with measles increases the epidemiological evidence at diagnosis.[citation needed]
There is no specific treatment or antiviral therapy for measles. Most patients will recover without complications with rest and supportive treatment.[citation needed]
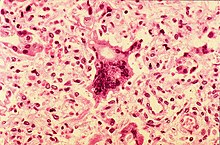
Some patients will develop pneumonia as a sequel to measles. Histologically, a single cell can be found in the paracortical region of the hyperplastic lymph nodes of patients affected by this condition. This cell, known as the Warthin-Finkeldey cell, is a giant multinucleotide cell with eosinophilic cytoplasm and nuclear inclusions. Those who have had an active measles infection or who have received the measles vaccine acquire permanent immunity against this condition.[citation needed]
The differential diagnosis between measles and Zika fever should be established.
Transmission
Measles is a highly contagious airborne virus that spreads primarily through the respiratory system. The virus is transmitted in respiratory secretions, and can be passed from person to person via droplets of saliva (Flügge droplets) that contain virus particles, such as those produced by a coughing patient. Once transmission occurs, the virus infects the epithelial cells of its new host, and can replicate in the urinary tract, lymphatic system, conjunctiva, blood vessels, and central nervous system.
Complications
Complications with measles are relatively common, ranging from the usual mild diarrhea to pneumonia, encephalitis, corneal ulceration leading to corneal abrasion. Complications are generally more severe in adults who are infected by the virus.
The percentage of fatal cases is approximately one death per thousand cases. In developing countries with high levels of malnutrition and poor health services, where measles is most common, the number of deaths is about 10 percent. In immunocompromised patients, the percentage increases to approximately 30 percent.[citation needed]
A rare but extremely serious complication is the so-called subacute sclerosing panencephalitis (SEEP), whose incidence is 7/1000 measles cases. Although in developed countries it is minimal and very few cases are diagnosed each year, it usually appears about 7 years after measles and is more prevalent in children who were first affected before the age of 2. It occurs when a defective virus, that is, whose synthesis of M protein is decreased, survives in brain cells and acts as a slow virus. Its symptoms are personality changes, behavior and memory changes, followed by sudden fasciculated contractions, as well as blindness. It is usually fatal.
Immunization and public health
Measles is a significant infectious disease because, although the complication rate is not high, the disease itself is so infectious that the large number of people who would suffer complications in an outbreak among non-immune people would quickly saturate the data. hospital resources available. If vaccination rates fall, the number of non-immune people in a community increases, thus the risk of a measles outbreak increases.
In developed countries, most children are immunized against measles by the age of 12 months, usually as part of the MMR (measles, mumps, and rubella) tripleviral vaccine. Vaccination is not applied before as children under 12 months retain anti-measles immunoglobulins (antibodies) transmitted from the mother during pregnancy. A booster shot should be received between four and five years of age. Vaccination rates have been high enough to make measles relatively rare. Even a single case in a college dorm room, or similar setting, triggers a local vaccination program, should any of the exposed individuals not be immune.[citation needed]
Unvaccinated populations face constant risk of disease. After vaccination rates dropped in northern Nigeria in the early 2000s due to political and religious objections, the number of cases rose significantly, and hundreds of children died. In 2005, an outbreak of measles in Indiana was attributed to children whose parents refused vaccination. In the early 2000s, the MMR vaccine controversy in the UK regarding a potential link between the combined MMR vaccine and autism led to a return of & 'Measles parties', in which parents deliberately infect children with measles to boost the child's immunity without an injection. This practice poses many risks to the child's health, and has been discouraged by public health authorities. Scientific evidence does not provide support for the hypothesis that MTS is a cause of autism. Declining immunization rates in the United Kingdom are the likely cause of a significant increase in measles cases, showing a steady increase in the number of cases.
According to the World Health Organization (WHO), measles is one of the leading causes of death among young children.
Globally, the death rate has been significantly reduced by signatories to the Measles Initiative: the American Red Cross, the US Centers for Disease Control and Prevention (CDC), the United Nations Foundation Nations, Unicef and the World Health Organization (WHO). Globally, measles deaths have fallen by 60%, from approximately 873,000 deaths in 1999 to 345,000 in 2005. Africa is the region that has shown the greatest progress, with a 75 percent reduction in annual measles deaths in just five years, from about 506,000 to about 126,000.
The press release released jointly by the Measles Initiative sheds light on another benefit of the fight against measles: "Measles vaccination campaigns are helping to reduce child deaths from other causes. They have become a channel for the delivery of other life-saving supplies, such as bed nets to protect against malaria, deworming medicine, and vitamin A supplements. Combining measles immunization with other health supplements is a contribution to the achievement of Millennium Goal #4: a two-thirds reduction in child deaths between 1990 and 2015."
Once the disease is contracted and cured, the body acquires permanent immunity.[citation needed]
Global eradication and resurgence
In 2007, Japan became a hotbed for measles. Japan suffered from a record number of cases, and a number of universities and other institutions in the country closed in an attempt to contain the outbreak.
In the 1990s, the American governments, together with the Pan American Health Organization, launched a plan to eradicate the three diseases that MMR is good for—measles, mumps, and rubella—from the region. [citation required]
Endemic measles has been eliminated from North, Central and South America; the last endemic case in the region was reported on November 12, 2002. In 2016, the American continent was the first—and the only, so far—in the world to have eliminated the disease.
Either way, outbreaks continue to occur following the importation of measles viruses from other world regions. For example, in June 2006, there was an outbreak in Boston that resulted from a resident traveling to India. In 2005, there was another outbreak in an unimmunized population of Indiana and Illinois, transmitted by an Indiana girl. who visited Romania without having been vaccinated. In Michigan, in the fall of 2007, a confirmed case of measles occurred in a girl who had been vaccinated and who apparently contracted it abroad. There were at least six other suspected cases, all among children who had been vaccinated.{Cr}}
In August 2010, cases of measles were reported in Argentina, in the province of Buenos Aires and in the Autonomous City of Buenos Aires, which are presumed to have been infected by people who attended the Soccer World Cup in South Africa 2010.[citation required]
During 2018, measles reappeared in Argentina, after 18 years of eradicating the disease, in 2000: the first was an autochthonous case in the country, in the city of Buenos Aires, and it spread to the province of the same name.
In August 2018, in Ecuador, after more than eight years of eradicating vernacular measles in the country, it reappeared with 19 cases, all of them imported by immigrants.
In August and September 2011, seven cases were confirmed in Barranquilla, Colombia, after many years without outbreaks of the disease. The Colombian government began a vaccination plan of eight million doses in the main cities of the coast and in Bogotá. According to government statements, it was due to the transit of foreigners, as a result of the 2011 FIFA U-20 World Cup Colombia.[citation required]
Although smaller organizations have proposed a global eradication of measles, mumps, and rubella, there are no serious plans yet, at least until the global eradication of polio.[quote required]
In late December 2014, a measles outbreak began in the United States; it is estimated that it took place when five people fell ill after visiting the Disneyland park. The Disney company reported that at least five employees fell ill with measles. This epidemic is the worst that has occurred in 15 years and, according to the media, it seems to be getting worse. Although the disease had been eradicated from the United States in 2000 According to the Center for Disease Control and Prevention of the United States, since the outbreak that occurred in Disneyland in December 2014, 644 cases were diagnosed in 27 states of that country, which caused the then president, Barack Obama, to ask the population to vaccinate their children. Two cases were reported in Argentina in 2018, which are still under investigation.
Controversy with anti-vaccine groups
Since vaccination began in the late 18th century, opponents have claimed that vaccines don't work, that they are or can be dangerous, that emphasis should be placed on personal hygiene instead, or that mandatory vaccinations violate individual rights or religious principles.[citation required]
It is difficult to be certain, but the reappearance of measles cases in developed countries such as the United States, Italy, the United Kingdom and Ireland lead us to suspect that the lack of vaccination promoted in the 2000s by anti-vaccine groups has favored this situation.
Measles reappeared in 2019 in the United States. Since January, 22 states in the country added a total of 695 cases of measles, a disease that was believed to have been eradicated almost more than two decades ago, when an outbreak of more than 30,000 cases emerged. From there, vaccination was promoted to all people.
The appearance of measles has been attributed to people not getting vaccinated. The disease is spreading in and around the United States. Measles outbreak data has been collected in: New York, Washington, New Jersey, California, Michigan.[citation needed]
People who do not accept vaccination against this disease put their health and that of everyone around them at risk, because according to Unicef, measles is more contagious than Ebola, tuberculosis or the flu. The contagion of this disease is very ferocious, as it can appear up to two hours after maintaining contact with an infected person. Furthermore, this disease is so contagious that it spreads through the air and infects the respiratory system. If measles is added to other damage to human health, such as malnutrition, it can kill them or unvaccinated babies. When contagion occurs, there is no specific treatment for the cure, so vaccination is essential to save people from this disease, especially children.
The five countries with the most cases against measles vaccination between 2010 and 2017 have been: the United States, with a figure of 2,593,000 people; 608,000 in France; United Kingdom, with 527,000 people; Argentina, with 438,000, and Italy, with 435,000 people.
In 2019, the World Health Organization listed these radicalized groups as one of the main threats to global health.
In 2020, measles outbreaks emerged in Mexico.
Contenido relacionado
Diogenes
Olaus Wormius
Hippocratic Oath
Manuel Amador Guerrero
Endocardium