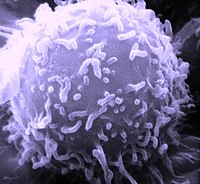
Lymphocyte
Lymphocytes are cells of the immune system. They are a type of leukocyte that come from the lymphoid differentiation of hematopoietic stem cells located in the bone marrow and that complete their development in the primary and secondary lymphoid organs (bone marrow, thymus, spleen, lymph nodes, and lymphoid tissues associated with the mucosa).). Lymphocytes circulate throughout the body through the circulatory system and the lymphatic system.
They are the smallest leukocytes (between 9 and 18 μm), and represent approximately 30% (20 to 40%) of the total in peripheral blood. Their morphology is variable, according to which they are classified as lymphoblasts, prolymphocytes, and lymphocytes as such, either inactive or activated (such as plasma cells). They present a large spherical nucleus that stains violet-blue and the amount of cytoplasm varies from scant (most frequent situation, in which the cytoplasm is observed as a blue peripheral ring) to abundant. In the cytoplasm are some mitochondria, free ribosomes, and a small Golgi apparatus.
The main function of lymphocytes is the regulation of the adaptive (or specific) immune response, reacting against foreign materials (microorganisms, tumor cells or antigens in general). To do this, they differentiate into three reactive cell lines: T lymphocytes that develop in the thymus and participate in the cellular immune response; B lymphocytes, which develop in the bone marrow and then migrate to different lymphatic tissues, which are responsible for the humoral immune response, transforming into plasma cells that produce antibodies; and NK (natural killer) cells that destroy infected cells. T and B lymphocytes have specific receptors, natural killer (NK) cells do not.
These cells are located mainly in the lymph and lymphoid organs and in the blood. They have receptors for specific antigens and can therefore be responsible for the production of antibodies and the destruction of abnormal cells. These responses occur within the lymphoid organs, which, for this purpose, must provide an environment that allows efficient interaction between lymphocytes, macrophages, and foreign antigen.
Types

1. Invasive/antigenic protein
2. Macrophagus/Antigen Submiting Cell
3. Antigen Complex:MHC II (Antigen Presentation), Th lymphocyte Activation
4. Lymphocyte Th (cooperator)
5. Invasive protein attached to membrane antibodies
6. Lymphocyte B
7. Antigen processing (MHC type II)
8. Antigenic Complex:MHC II (Antigen Representation)
9. Production of antigen-specific antibodies
10. Activation of B lymphocytes with activated Ths.
The typology of lymphocytes is difficult to classify according to their morphology, so properties such as reactivity to monoclonal antibodies that identify their "CD" or clusters of differentiation (from the English cluster of differentiation), which are a set of biological markers for cell identification; the reconfiguration status of immunoglobulin heavy chain and light chain genes or T and B cell receptors; and the expression of immunoglobulins on the surface.
B lymphocytes
B lymphocytes mature in two stages: the first, without mediating antigens, which occurs in the bone marrow, and the other, dependent on exposure to antigens, which occurs in secondary lymphatic organs (lymph nodes, spleen, and lymphoid tissues associated with the mucosa) where they are transformed into cells that produce and secrete antibodies. The different types of B lymphocytes in these stages are:
- Pro-B stadium.
- Pre-B stage.
- B immature lymphocytes.
- Mature B lymphocytes.
Lymphocytes are responsible for the humoral response, transforming into plasma cells that produce glycoproteins called antibodies or immunoglobulins (Ig), which adhere to a specific antigen (which they recognize univocally).. All antibodies produced by a B lymphocyte are specific for a single antigen, which is why such antibodies are called monoclonal. B lymphocytes also interact with T lymphocytes, thereby proliferating and changing the immunoglobulin isotype (IgM, IgE, IgG, IgD, IgA) that they secrete, maintaining antigen specificity. Also B lymphocytes can act as antigen presenting cells.
T lymphocytes
T lymphocytes (thymus-dependent, since they differentiate in the thymus): They detect protein antigens associated with molecules of the major histocompatibility complex (MHC or MHC)
- CD4+ lymphocytes T collaborators (in English "helper") or CD4+ lymphocytes. They recognize antigen peptides presented by MHC-II in dendritic cells, B lymphocytes, macrophages and other antigen-representative cells. They are called collaborators because they are involved in the activation and direction of other immune cells.
- Cytotoxic T lymphocytes or CD8+ lymphocytes. They recognize peptides presented by MHC-I and have liptical capacity.
- Lymphocytes T regulators or suppressors that inhibit the production of interleucins of T collaborator lymphocytes and therefore stop the specific immune response.
- Memory T lymphocytes that after first contact with an antigen remain as memory cells for many years and that if a second contact was produced they would produce cytotoxic T lymphocytes and collaborators quickly.
NK cells
- Natural Killer Cell, Natural Killer or large granular lymphocyte: They play a role very similar to that of cytotoxic T lymphocytes in the adaptive autoimmune response of our organism. A NK cell will act immediately in the presence of an antigen, while a cytotoxic T lymphocyte will need the immune response to activate. A Natural killer does not need antibodies to target cells affected by the antigen, but will be able to recognize them immediately to destroy them.
NK cells fight the antigen present on the infected or cancer cell immediately; meanwhile the adaptive immune response is generating specific cytotoxic T cells, to kill off those cells in a second step.
Lymphocyte trafficking
Trafficking lymphocytes between tissues, the bloodstream, and lymph nodes allows cells sensitive to antigens to seek out and be recruited to sites where a response is developing. In turn, there is a dissemination of memory cells that allows the organization of a broader response.
- After the first 24 hours (in which the antigen is first located in the lymph nodes or spleen) the reactive cells to the antigen suffer a depletion (decrease) of the surrounding lymphocytes.
- Days later (after the proliferation of antigen at the location site), a peak of active cells appears in the chest duct.
- In the efferent lymphatics there will be a fall in cell production, a phenomenon designated as “cell lock” or “ lymphocyte catch” that is believed to be the result of the release of soluble factors from T cells induced by the antigen, this event will be followed by a production of activated blasts that reaches a maximum of 80 hours.
- Virgin lymphocytes enter the lymph node through the affluent lymphatic and through the guided passage through the high-wall endothelium of the specialized postcapills.
- Endotelios of this type allow the transit of cells linked in the immunity of mucosas to Peyer plates; they also involve the migration of lymphocytes in normal and swollen tissues.
- Lymphocytes join unskilled flat endothelials and cross them.
- Lymphoblasts and populations of memory cells show a limited migration to tissue to extralyphoid tissues, such as skin or mucous epithelium; while lymphocytes, neutrophils and monoliths are directed and migrated to inflammation sites in response to locally produced mediators.
- Traffic and recirculation of lymphocytes through encapsulated lymphoid tissue and inflammation sites: Blood-borne lymphocytes enter the lymph nodes and tissues through the high-wall endothelium of the post-capill (HEV) cells and go through drainage lymphatics. Eferent lymphatics, coming out from the last node, join in forming the thoracic duct by which blood lymphocytes return. In the spleen, which lacks HEV, lymphocytes enter the lymphoid area (white pulp) from the arterioles and pass to the synusoids of the eritroid area (red pulp) and go out splenicly.
- Traffic and circulation of lymphocytes within the lymphoid system associated with mucosa-not encapsulated (MALT): Cells stimulated by an antigen move from Peyer's plates, move to colonize their own foil and other mucous membranes, and form a common mucous immune system.
- This organized traffic is carried out by directing the relevant lymphocytes to different parts of the lymphoid system and other tissues, through a series of guide receptors that include: members of the superfamily of the integrains (LFA-1, VLA, etc.) and a member of the suplefamily of the selectins, which is the L-selectine.
Integrins can bind to the extracellular matrix, plasma proteins and other cell surface molecules, their complementary ligands include vascular surface addressins, present on the endothelium of blood vessels.
These guide receptors act as selective gates that allow particular populations of lymphocytes to gain access to the appropriate tissue.
Chemokines such as SLC (secondary lymphoid tissue chemokine) presented by the vascular endothelium, have an important role for the detection of lymphocytes; integrin receptors are involved in the functional upregulation of integrins.
Transmigration
- Step No. 1 - Adherence and rotation: In order for the lymphocyte to adhere to the endothelial cell, it must overcome the clutch forces created by the blood flow. This is achieved by means of a force of attraction between the guide receptors (integrines and L-selectine) and their ligands on the wall of the vessel that operates through microvellosities on the surface of the lymphocyte. After this adhesion process; the lymphocyte rotates along the endothelial cell and the VLA-4 or LPAM-1 in the lymphocyte, join their ligands on the endothelio.
- Step No. 2 - Activation of LFA-1 and flattening: This process leads to the activation and recruitment of the LFA-1 integration into the non-very surface of the lymphocyte. This integraline binds heavily to ICAM-1 and ICAM-2 on the endothelial cell, and intimate contact makes the lymphocyte flat.
- Step No. 3 - Diapedesis: The flat lymphocyte now uses the LFA-1-ICAM interaction and the member of the PECAM-1 immunoglobulin superfamily (platelet adhesion molecule, CD31, not only present in the platelets), to open the way between the endothelial cells and the tissue, in response to a chemotactic signal.
Pathology
Lymphocytosis
The normal proportion of lymphocytes within all leukocytes varies between 20 and 40%, and therefore, a proportion that exceeds 40% would determine a relative lymphocytosis.
Lymphocytopenia
Lymphocytopenia is used to refer to an abnormally low level of lymphocytes in the blood.
Contenido relacionado
Cyclocarpales
Capparaceae
Araliaceae