Lyme's desease
Lyme disease (also known as Lyme borreliosis) is an infectious disease caused by some of the bacteria of the genus Borrelia, transmitted by ticks. The disease can affect the skin, nervous system, heart, joints, and muscles; the affectation varies according to the species of Borrelia causing it.
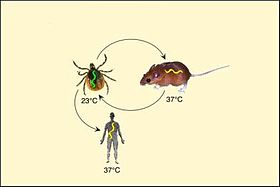
It is a zoonosis, since it is naturally transmitted to humans from the animals that act as a reservoir of the spirochete, mainly wild rodents and cervids.[citation required] It is the most prevalent tick-borne disease, being endemic in several states in the eastern and southwestern United States and in some European countries.[citation needed] The The disease is caused by three species of spirochetes of the genus Borrelia; B. burgdorferi, Borrelia afzelii and Borrelia garinii. They are transmitted to humans by ticks of the genus Ixodes: in Europe, mainly by Ixodes ricinus, to a lesser extent by I. persulcatus, and in North America generally by I. scapularis.[citation needed]
The most common and distinctive sign of an acute infection is a target-shaped skin rash, known as erythema migrans, which appears at the site of the tick bite, approximately one week later. The rash is rarely itchy or painful, so it is not always detected. Approximately 70–80% of infected people show this diagnostic sign. Other early manifestations may include fever, headache, and fatigue If left untreated, it can progress to facial paralysis, joint pain, severe headaches with a stiff neck or heart palpitations, among others.
Description
The first descriptions of Lyme disease were made in 1883 by Alfred Burchwald, in 1902 by Karl Herxheimer and Kuno Hartmann and in 1909 by Benjamin Lipschutz and Arvid Afzelius; the latter described chronic erythema migrans in Europe. A year later, Afzelius described the association of these lesions with a tick bite.
Between 1975 and 1977, a total of 51 patients with the presumed diagnosis of juvenile rheumatoid arthritis were studied in residents of three contiguous communities in the US state of Connecticut: Old Lyme, Lyme, and East Haddam. The researchers fully described the infection as well as its association with a vector, naming the disease after the Lyme locality.
Between 1981 and 1982 Burgdorfer isolated and identified the causative microorganism within the gastrointestinal tract of the Ixodes tick, concluding that it was a spirochete of the genus Borrelia, which was called B. burgdorferi in honor of its discoverer.
Epidemiology
The epidemiology of Lyme borreliosis is complex, based on interactions between the pathogen (B. burgdorferi sensu lato), the vector (ticks Ixodes spp.) and the vertebrates that act as reservoirs.
Population movements, outdoor activities, leisure or work, agroecological and climate changes can modify its distribution and prevalence, and it is currently discussed whether they are increasing.
In Europe
In many European countries Lyme disease is endemic; its prevalence is 4%. Some people may be asymptomatic carriers. Its highest prevalence is observed in Central and Eastern European countries. In Austria and Slovenia there are between 120 and 130 cases per 100,000 inhabitants. The infection occurs mainly in spring, summer and early autumn, due to the life cycle of ticks, whose larvae emerge in spring, fixing themselves on small vertebrates, their first hosts, from which they can become infected with spirochetes. By the following spring, these larvae have developed into nymphs, which before feeding are very small and unnoticed. Their small size makes them inconspicuous, but infected nymphs can effectively transmit the infection to humans.
In America
In the United States, between 1992 and 2006, the reporting of new cases of Lyme disease doubled (from 9,908 to 19,931 cases per year). It occurs mainly in males, either between five and nine years; or, between 55 and 59 years.
The American CDC (Centers for Disease Control and Prevention) publishes an annual map with the incidence, according to the notifications received. It shows that the incidence is very heterogeneous and is only endemic in the northeast of the country.
In Mexico, the prevalence is 1.1%.
Etiology
Lyme disease is caused by several species of the genus Borrelia: B. burgdorferi, B afzelii and B. garinii. They are gram-negative spirochetes with anaerobic metabolism.
To produce the infection, the tick must attach itself to the host for at least 36 hours and fatten, since B. burgdorferi takes 36 to 48 hours to migrate from the stomach to the salivary glands of the parasite, as long as it has fattened.
Pathogenesis
Lyme disease belongs to a group of pathologies in which vascular damage and neurotropism are common: in infections by Rickettsia, Borrelia, Coxiella . Granulomatous lesions and endothelial cell tropism occur in Bartonella and Francisella infections. Unlike Lyme borreliosis, another disease in this group, Mediterranean boutonniere in its malignant form can cause death. If Borrelia burgdorferi infection is not detected in its primary state, it can cause chronic neurological manifestations.[citation needed]
Clinical picture
Lyme disease can have up to four stages, or states. Not all are always observed, and there is insufficient evidence that primary infection always progresses to secondary, late, and chronic stages.
According to the Asbrink and Hovmark classification, Lyme disease has two stages: early borreliosis (localized and disseminated) and late borreliosis.
Early localized Lyme disease
Between 50 and 80% of people with early Lyme disease develop the most characteristic sign of the disease, called erythema migrans. It is a macular eruption, which appears between one to two weeks (range between 3 to 30 days) after the bite, generally on the lower extremities (54%) or on the trunk (29%). The eruption spreads slowly, clearing in the center, exceeding 5 cm in diameter, with an average of 16 cm (the largest described measured 70 cm); Between 10 to 20% of cases present multiple lesions. His resolution is spontaneous. This lesion is considered pathognomonic of the disease.
Associated symptoms are similar to those of a non-specific viral infection: fatigue, malaise, fever, chills, myalgia, and headache.
Early Disseminated Lyme Disease
In this phase of the disease, which manifests weeks to months after infection, the heart, skin, musculoskeletal system, and nervous system may be affected.
- Heart: one to two months after infection (range between one to seven months) a carditis is presented in 4 to 10 % of patients whose manifestations include: chest pain, exercise dyspnea, tiredness, palpitations, syncope and some forms of atrioventricular block. They may also occur in less common pericarditis, branch blockages and heart failure.
- Skin: Persistent Multiple Erythema.
- Musculoskeletal: osteoarticular pain (myalgias and artralgias) is a common manifestation of this stage.
- Nervous system: up to 15% of patients have lymphocytic meningitis, cranial neuropathies (such as facial paralysis), radiculopathy, multiple mononeuritis, cerebellar ataxia and myelitis. Patients are presented with language impairment, blurred vision, clumsy movements, hallucinations and facial paralysis due to facial nerve involvement.
Late Lyme Disease
Late-stage Lyme disease can occur months or even years after the initial stage. It presents with skeletal and neurological disorders.
- Arthritis, which appears about 6 months after infection, mainly from knees and hips, from one or more joints, with pain and swelling that can acquire a chronic course.
- Subacute encephalopathy, encephalomyelitis or axonal polyneuropathy.
In addition to the aforementioned symptoms, more serious neurological disorders (confusion, sleep disorders, memory loss) can be added. Skin signs such as chronic atrophic acrodermitis may appear at this stage.
“Chronic Lyme”
The name chronic Lyme disease or chronic lyme disease —Chronic Lyme disease, CLD— is used by some therapists, mainly from alternative practices, to refer to pictures of fatigue, muscle or joint pain, attributing them to a Lyme disease that does not respond to treatment or that has not been diagnosed. Most microbiologists criticize this name, arguing that the symptoms and signs attributed to "chronic lyme" can occur both in subacute forms of lyme and in other different diseases.
Symptoms that persist after treatment are called Post-Treatment Lyme Syndrome, and are a known sequelae, although their cause is unclear. Also, the sometimes non-specific symptoms of Lyme disease are an argument used to convince that any picture of fatigue and muscle pain is, in reality, undiagnosed or chronic Lyme disease, which can end in misdiagnosis and misdiagnosis. unnecessary, ineffective, expensive, and dangerous treatment. Victims are hypochondriacs, or suffer from other, often disabling, diseases such as ME-CFS, fibromyalgia, or some forms of multiple sclerosis.
Many people are diagnosed with chronic Lyme despite negative tests for Borrelia burgdorferi, and they may not even have been exposed to a situation that would lead to suspicion of contagion.
Diagnosis
Clinical diagnosis is made on the basis of observation of erythema migrans. In endemic areas, this sign should prompt adequate treatment. In non-endemic areas, differential diagnoses such as erythema multiforme, granuloma annulare, hypersensitivity dermatitis, staphylococcal infections, nummular eczema, spider bite, ringworm, or urticaria should be considered.
Simple serologic tests have been shown in many studies to give false negatives and false positives, so diagnosis must combine serologic tests with clinical signs. Among the diseases that can produce false positives are: syphilis, brucellosis, infectious mononucleosis, mumps, and rheumatic diseases such as lupus.
The CDC recommends a two-stage serologic test, consisting of two successive assays: a highly sensitive immunofluorescence assay (IFA) or enzyme-linked immunosorbent assay (ELISA), followed, if positive, by a known specific test. as Western blot, which confirms it. If the ELISA yields a negative result, it is not necessary to confirm, since its sensitivity is high. Diagnosis by direct visualization of spirochetes in tissue or culture also has difficulties, so both these and PCR from clinical samples are recommended only in certain rare circumstances.
Application and interpretation guidelines adapted to European Borrelia species have been published in the European Union. The Conformité Européene (CE) standard provides a minimum standard for commercial diagnostic kits.
Diagnostic tests not recommended
Some laboratories offer Lyme disease testing using assays whose accuracy and clinical utility have not been adequately established. Examples of non-validated tests include:
- Antigen screening tests in the urine.
- Cultivation, staining by immunofluorescence or counting of cystic forms or with incomplete cell wall of B. burgdorferi.
- Lymphocyte transformation tests.
- Quantitative tests of CD57 lymphocytes.
- "Reverse Western blots".
- Own criteria for the interpretation of immunotransfers.
- Measurement of antibodies in joint fluid (synovial fluid).
- IgM or IgG tests without an ELISA / EIA / previous IFA.
Treatment
The treatment consists of the application of antibiotics, which vary depending on the state of the disease, and the age of the patient. Ibuprofen is also often given to relieve inflammation. Early indication, in the localized early stage, allows the vast majority of cases to be completely resolved.
Treatment of early infection (local or disseminated) consists of large doses of oral antibiotics, where doxycycline (100 mg p.o./12 h), for 10-14 days, is the treatment of choice, although amoxicillin (500 mg p.o./8 h) for 14-21 days could also be used, if it is a child or a pregnant woman.
The prognosis is usually positive, however, arthritis symptoms may persist.
For the treatment of the late disseminated phase of the disease, ceftriaxone is generally used in higher doses (2 g IV/24 h for 14-28 days) than for the primary stage, although cefotaxime (2 g i.v./8 h for 14-28 days) or penicillin G sodium could also be given.
Prophylaxis
Developing vaccines to prevent Lyme disease is challenging. This is because the bacteria that cause the disease have highly variable antigens and their expression levels also vary depending on the host in which they are found.
Currently, there is no effective vaccine for Lyme disease, but the main antigens on which the studies are based are the lipoproteins OspA and OspC. OspA is a protein that is highly expressed in Borrellia while it is in the intestine of ticks, but once it infects the blood its levels decrease and those of OspC increase. It is thought that OspA could be responsible for the adhesion of the bacteria to the intestine of ticks and OspC would be in charge of the migration of the bacteria towards the salivary glands, and of the infection in vertebrates.
In this way, vaccines with the OspA antigen began to be produced, which would induce the production of anti-OspA antibodies and, when found in the blood ingested by the insect, would neutralize the bacteria in the intestine of the tick, preventing its transmission. However, those bacteria that were already found in the salivary glands could be transmitted. In addition, another problem in the administration of the OspA lipoprotein is its similarity to a lymphocyte protein (hLFA-1), which could cause the appearance of autoantibodies. For this reason, attempts are being made to generate recombinant OspA proteins that do not generate autoimmunity. These recombinant proteins have been designed with regions of the OspA protein from bacteria with different serotypes, since, although the OspA protein is more conserved between species than OspC, one of the main problems is that the vaccine is effective against very few serotypes.
Alternatively, ticks are also the target of potential vaccines that would prevent them from being infected by pathogens, or, alternatively, from parasitizing humans.
LYMErix
In December 1998, the pharmaceutical company SmithKline Beecham, —currently GlaxoSmithKline— put on sale a vaccine called «LYMErix», manufactured with 30 μg of recombinant lipoprotein OspA. However, a few years later the vaccine was withdrawn when it was shown that it had several limitations: due to the need to administer three doses spread over 12 months, the acquisition of immunity was delayed by one year; the vaccine only protected against Lyme borreliosis caused by Borrelia species present in North America; and long-term protection proved short-lived. This, together with the difficulty of proving its safety in children under 15 years of age —a population with a higher risk of acquiring the disease—, led to its being voluntarily withdrawn from the market in February 2002.
Valneva
In July 2017, Valneva, an Austrian pharmaceutical company, received authorization from the US FDA to start a phase I study of a vaccine based on a recombinant OspA protein, called VLA15. This first study assessed the efficacy of different antigen dosages and their combination with or without adjuvant. The good results have allowed the start of phase II, the publication of which is scheduled for mid-2020.
Contenido relacionado
Psoas minor muscle
Benzopyrene
Aorta