Lung cancer
Lung cancer is a group of diseases resulting from the malignant growth of cells of the respiratory tract, particularly lung tissue, and one of the most frequent types of cancer worldwide. Lung cancer usually originates from epithelial cells, and can lead to metastasis and infiltration into other body tissues. Neoplasms that metastasize to the lung from tumors in other parts of the body are excluded from lung cancer.
The most common symptoms are shortness of breath, coughing, including bloody coughing, and weight loss, as well as chest pain, hoarseness, and swelling in the neck and face.
Lung cancer is classified into two main types based on the size and appearance of the malignant cells: small cell (small cell) lung cancer and non-small cell (non-small cell) lung cancer. This distinction conditions the treatment and thus, while the former is generally treated with chemotherapy and radiation, the latter also tends to be treated by surgery, laser, and, in select cases, photodynamic therapy.
The most common cause of lung cancer is smoking, with 95% of lung cancer patients being current or former smokers. In non-smokers, the development of lung cancer is the result of a combination of genetic factors, exposure to radon gas, asbestos, and air pollution, including secondhand smoke (passive smoke).
Early diagnosis of lung cancer is the main determining factor for successful treatment. In early stages, lung cancer can, in around 20% of cases, be treated by surgical resection with successful cure. However, due to its virulence and the difficulty of early detection, in most cases In most cases, the diagnosis occurs when metastasis already occurs; Lung cancer presents, along with cancers of the liver, pancreas, and esophagus, the worst prognoses, with an average life expectancy of approximately 8 months.
Lung cancer is one of the most serious diseases and one of the cancers with the highest incidence in humans, responsible for the highest cancer mortality rates worldwide. It is the leading cause of cancer mortality in the world. male and the third, after colon and breast, in women, causing more than a million deaths each year in the world. In the United Kingdom (2004) and in the United States (2006) it represents the first cause of cancer death in women and men. In Spain, some 20,000 cases are diagnosed annually, which represents 18.4% of the tumors among men (18,000 cases) and 3.2% among women (2,000 cases). Despite the difficulty in To find consistent statistics among the different countries of Ibero-America and the Caribbean, overall survival has been increasing, especially in patients undergoing regular chemotherapy treatment.
History
Lung cancer was very rare before the spread of smoking and, at least until 1791 with John Hill's reports, it was not considered a major disease entity. the salient features of lung cancer, a disease then difficult to distinguish from tuberculosis. By 1878 malignant lung findings accounted for only 1% of cancers observed during autopsies. The figure rose to 10–15% in the first part of the XX century. Up to 1912 there were only 374 cases published in the medical literature on cancer of the lung. In 1926, small cell lung cancer was first recognized as a malignant disease entity, unlike all other types of lung cancer. Reviewing these studies demonstrates an increased incidence of lung cancer at autopsy from 0.3% in 1852 to 5.66% in 1952.
German physician Fritz Lickint reported the first statistical evidence linking lung cancer to cigarette smoking in 1929, which led to an impressive anti-smoking campaign in Nazi Germany. A study, begun in the 1950s by British physicians, detected the first strong evidence epidemiological connection between smoking and lung cancer. As a result, in 1964, the United States began public campaigns about the harmful effects of cigarette smoking.
The radon connection was first recognized in the Ore Mountains region around Schneeberg, in the border area between Saxony (Germany) and Bohemia (Czech Republic). This region is very rich in fluorite, iron, copper, cobalt and silver, the latter mined since the 1470s. The presence of large amounts of uranium and radium led to intense and continuous exposure to radon, a radioactive gas with properties carcinogenic.
The miners developed a disproportionate number of lung diseases which, on epidemiological follow-up, led in the 1870s to the discovery of certain varied and by then unreported disorders, which coincided with the characteristics of lung cancer described years later. It is estimated that around 75% of these miners died of lung cancer. Despite this discovery, uranium mining in the Soviet Union continued even into the 1950s, due to continued demand for the metal.
The first successful pneumonectomy operation for lung carcinoma was performed on April 5, 1933. Radiation therapy in palliative care cases has been used since the 1940s, while radical radiation therapy (an attempted radiation at higher doses) began to be used from the 1950s onwards as therapeutics in people with lung cancer, but without an indication for surgery. In 1997, continuous accelerated hyperfractionated radiotherapy (CHART) supplanted radical conventional radiotherapy for lung cancer.
For small cell lung cancer, early surgical approaches in the 1960s and radical radiation therapy have yielded disappointing results. Successful chemotherapy regimens were not developed until the 1970s.
Classification
| Histological form | Frequency (%) |
|---|---|
| Non-small cell lung cancer | 75-80 |
| Small cell lung cancer | 15-20 |
| Carcinoid | . |
| Unspecified lung cancer | . 2 |
| Sarcoma | 1 |
The vast majority of lung cancers are carcinomas, that is, malignant tumors that arise from epithelial cells. There are two forms of lung carcinoma, categorized by the size and appearance of the malignant cells seen histopathologically under a microscope: non-small cell (80.4%) and small cell tumors. small (16.8%). This classification is based on histological criteria and has important implications for the treatment and prognosis of the disease. Non-small cell carcinomas can be divided, with the aid of a microscope, into several major classes: adenocarcinomas, squamous cell carcinomas, and large cell carcinomas. There are also bronchoalveolar carcinomas and various mixed forms.
Non-Small Cell Lung Cancer (NSCLC)
Non-small cell lung carcinomas are grouped together because their prognosis and treatment are very similar. There are three main subtypes: squamous cell carcinoma of the lung, adenocarcinomas, and large cell lung carcinoma.
| Histologic subtype | Frequency (%) | |
|---|---|---|
| Squamous cell lung carcinoma | 31.1 | |
| Adenocarcinoma | Adenocarcinoma (not specified) | 23.2 |
| Carcinoma bronchioloalveolar | 3.0 | |
| Carcinoma adenoescamoso | 1.2 | |
| Adenocarcinoma papilar | 0.7 | |
| Mucoepidermoid carcinoma | 0.1 | |
| Carcinoma adenoid cystic | 0.04 | |
| Other adenocarcinomas | 1.1. | |
| Large cell carcinoma | 10.7 | |
| Carcinoma of giant and star cells | 0.4 | |
| Other or unspecified non-small cell type | 8.9 | |
About 31% of all lung carcinomas are squamous cell carcinoma, which usually begins near a central bronchus. Necrosis and cavitation are commonly seen in the center of the tumor. Well-differentiated squamous cell tumors often grow more slowly than other types of cancer.
Adenocarcinomas account for 29.4% of all types of lung cancer. They generally originate in peripheral lung tissue. Most cases of lung adenocarcinoma are associated with cigarette smoking and in patients with pre-existing lung disease. Among those who have never smoked, however, adenocarcinomas are the most common form of lung cancer. One of the subtypes of adenocarcinomas, bronchioloalveolar carcinoma, is seen more frequently among women than ever before. have smoked and generally show different responses to treatment from one individual to another.
Giant cell carcinomas account for 10.7% of all forms of lung cancer. They are rapidly growing tumors near the surface of the lung. They are often poorly differentiated cells and tend to metastasize early.
Small Cell Carcinoma (SCLC)
About 15% of all lung carcinomas are small cell lung cancer, also called oat cell carcinoma. It tends to occur in the larger airways. caliber—as in the primary and secondary bronchi—and grows rapidly to a large size. The oat cell contains dense neurosecretory granules, that is, vesicles that contain neuroendocrine hormones, giving it an association with an endocrine or paraneoplastic syndrome., that is, characterized by symptoms unrelated to the effect of the local tumor. Although it is a type of cancer that is initially more sensitive to chemotherapy, it carries a worse prognosis and spreads much more rapidly than non-small cell lung cancer. Small cell lung tumors are divided into a limited stage and an advanced or disseminated stage. This type of cancer is also associated with smoking.
Lung cancer metastasis
The lung is a common site for metastasis spread from tumors that start elsewhere in the body. The most common tumors that spread to the lungs are bladder cancer, breast cancer, colon cancer, neuroblastomas, prostate cancer, sarcomas and Wilms tumor. These are cancers identified by site of origin, so a breast cancer in the lung is still a breast cancer. They often have a characteristic rounded shape on chest x-ray. Primary lung tumors metastasize especially to the adrenal glands, liver, brain, and bone.
Epidemiology
Globally, lung cancer is the most common form of cancer in terms of incidence and mortality, causing about 1.0-1.18 million deaths each year, with the highest rates in European countries. and North America. The most affected population segment are those over 50 years of age who have a history of smoking. Lung cancer incidence by country is inversely correlated with exposure to sunlight or ultraviolet rays, suggesting that insufficient ultraviolet B light irradiation, leading to vitamin D deficiency, may contribute to cancer incidence. lung.
Frequency
Lung cancer or bronchogenic carcinoma represents more than 90% of lung tumors. Of this 90%, 93% correspond to primary lung cancer and 4% are secondary or metastatic tumors. 2% correspond to bronchial adenoma and 1% are benign tumors. The term bronchogenic is applied to most lung cancers, but is somewhat misleading as it implies a bronchial origin for all of them, despite the fact that adenocarcinomas, which are peripheral, are more frequently of bronchiolar origin. The relationship with smoking is such that the incidence of death from lung cancer is 46, 95, 108, 229 and 264 per 100,000 inhabitants among those who smoke half a box, ½-1 box, 1-2 boxes, 2 boxes and more than 2 daily cigarette boxes, respectively.
Mortality
Lung cancer is a very aggressive neoplasm: more than half of patients die within the first year after diagnosis, mainly because more than two thirds of individuals are diagnosed in advanced stages, when treatments are impossible curative. The most common cause of cancer-related death is lung cancer. In the United States, more people die from lung cancer than from colon, breast, and prostate cancer combined. While in other countries Like Venezuela, the number of deaths from lung cancer is surpassed by prostate cancer in men and breast cancer in women.
Increased incidence
The number of cases has been increasing since the early 20th century, doubling every 15 years. The incidence increased about 20-fold between 1940 and 1970. At the beginning of the XX century, most of the lung tumors were metastatic, and that primitive cancer was rare. Lung cancer is less common in developing countries, however the incidence is expected to increase markedly in the coming years in these countries, especially in China and India.
Sex
Lung cancer is the most frequent neoplasia in men, especially in Eastern Europe, with rates close to 70 cases per 100,000 inhabitants per year in the countries with the most cases, and a rate close to 20/ 100,000 in countries such as Colombia, Switzerland and other countries that report the lowest incidences. The rate among women is approximately half that of men, with rates close to 30 per 100,000 women per year in countries with more cases and a rate close to 20 in countries such as Colombia, Switzerland and other countries that report the lowest incidences. India has a rate of 12.1 and 3.8 per 100,000 among men and women respectively. having a lower incidence, but death from lung cancer has already ranked in some countries second only to breast cancer, even first. Although the death rate among men in Western countries is declining, the rate mortality of women due to lung cancer ón is increasing, due to the increase in the number of new smokers in this group.
Age
Lung cancer mostly affects people between the ages of 60 and 65. Less than 15% of cases occur in patients under 30 years of age. The average age of people diagnosed with lung cancer is 60 years. Since an increase in the rate of lung cancer has been observed in many countries, number of young smokers, changes in mortality by age will be observed in the coming decades.
Etiology or cause of lung cancer
The main causes of lung cancer, as well as cancer in general, include carcinogens such as cigarette smoke, ionizing radiation, and viral infections. Exposure to these agents causes changes in the DNA of the cells, progressively accumulating genetic alterations that transform the epithelium that lines the lung bronchi. As the damage becomes more extensive, the probability of developing cancer increases.
Smoking
It has been established that tobacco, and possibly air pollution, are a causative factor in lung cancer. Between 80-90% of lung cancers occur in smokers or in people who have quit smoking recently, but there is no evidence that smoking is associated with a particular histology, although it tends to be associated more with squamous cell carcinoma and small cell cancer. Statistically it is not associated with adenocarcinoma. Smokers have a 10 to 20 times greater risk of developing lung cancer (depending on the number of cigarettes smoked per day) than non-smokers. In other words, there is a linear dose-response relationship.
The more years of life a person has smoked and especially if it is at an early age, it is more related to cancer, since the dose of carcinogens is cumulative. For example, the risk increases between 60-70 times in a man who smokes two packs a day for 20 years, compared to a non-smoker. Although quitting smoking reduces the risk of developing lung cancer, it does not reduce it to the levels of never smokers. Even with quitting smoking, a high risk of lung cancer remains for the first 5 years. In most studies, the risk for ex-smokers approaches that of nonsmokers after 10 years, but may remain elevated even after 20 years. In a study conducted in Asturias (Spain), those who quit smoking 15 years before developing lung cancer had a 3 times higher risk than non-smokers.
A passive smoker is a person who does not smoke, but who breathes tobacco smoke from smokers, whether at home, at work, or in public places. The passive smoker has high levels of risk of contracting lung cancer, although lower in relation to the active smoker. The active smoker has the possibility of contracting a disease from tobacco in 80% of the cases, while in the smoker passive, the risk is 23%. There is no evidence to suggest that the risk of contracting lung cancer is higher in passive smokers than in active smokers.
Smoking cigars, cigars, or pipes is less likely to cause lung cancer than cigarette smoking even though the amount of carcinogens in pipe and cigar smoke is at least as great as in cigarette smoke.
Cultural groups that advocate non-smoking as part of their religion, such as Latter-day Saints and Seventh-day Adventists, have much lower rates of lung cancer and other cancers associated with smoking tobacco.
Tobacco is responsible for 30% of cancers in general and in decreasing order of frequency they are: lung, lip, tongue, floor of the mouth, pharynx, larynx, esophagus, urinary bladder and pancreas.
Comparison with Marijuana
A study comparing marijuana (741 to 985 mg) and tobacco (900 to 1,200 mg) cigarettes found that smoking marijuana tripled the amount of tar inhaled and increased the amount of tar deposited in the respiratory tract by one-third. Many of the cancer-causing substances in tobacco are not in the products of combustion of marijuana. Some medical reports indicate that these products of marijuana combustion will not cause mouth and throat cancer any more frequently than tobacco. However, because marijuana is an illegal substance, it is not easy to obtain information about the relationship that marijuana combustion products have with cancer on the basis of molecular, cellular, and histopathological grounds.
Endogenous factors: genetics and sex
Lung cancer, like other forms of cancer, is initiated by activation of oncogenes or inactivation of tumor suppressor genes. Oncogenes are genes that appear to make an individual more susceptible to cancer. For their part, proto-oncogenes tend to become oncogenes when exposed to certain carcinogens.
Several studies indicate that women have a higher risk of developing lung cancer than men for the same tobacco exposure. Siblings and children of people who have had lung cancer may have a slightly higher risk than men. the general population. If an individual's father and grandfather died from lung cancer and the individual smokes, the most likely cause of death is lung cancer.
No factor responsible for genetic susceptibility could be demonstrated. However, every day there is more evidence of the participation of genetic factors and other biomarkers of susceptibility in the predisposition to lung cancer, among them:
- The existence of a genetic factor linked to the aril-hydrocarbon-hydroxylase enzyme (AHH) which is an enzyme of benzopirene metabolism. AHH has been observed in some patients, an enzyme that has the ability to convert polycyclic hydrocarbons into highly carcinogenic substances. It has also been detected in other cases that the vitamin A deficiency could have a similar effect. Available data support the hypothesis that dietary carotenoids such as vitamin A reduce the risk of lung cancer, although they also suggest the possibility that some other factor in these foods is responsible for the lowest risk found.
- The existence of oncogenes activated in the tumor tissue of lung cancer has been shown. These include oncogene amplification myc in small cell tumors, punctual mutations in oncogene coding regions ras in different cell lines and specific mutational activations of oncogen K-ras in non-small cell tumors like adenocarcinomas. It is currently being studied whether the increases or alterations of the proteins expressed by these activated genes play some role in the pathogenic lung cancer.
- Cell or humoral immunity is a factor of susceptibility. So far it has not been clear whether immunodeficiency is prior to or secondary to neoplasm itself.
- Non-smokers with lung cancer have an increase in oncogen p53 variants with genotype Arg homozygous.
According to studies, it has been possible to define a classification within lung cancer based on the number of somatic copy mutations (SCNAs) that are visualized at the genomic level for lung cancer in non-smokers, being able to differentiate patients in:
- Piano: Individuals without mutations of SCNAs. These individuals tend to have better prognoses, especially those with carcinoids. Some of the mutations that may appear are associated with KRAS and UBA1 genes.
- Mezzo-forte: Individuals whose genes have chromosomal arm-level amplifications (1q, 5p, 7p, 7q and 8q). Modifications are often seen at the EGFR level (Receptor of the Epidermal Growth Factor).
- Forte: Individuals who present duplications at the level of the entire genome. The most common mutations are found in TP53. Most smokers are within this subgroup.
Although the previously established classification is determined for non-smokers, an association is seen between the genomic features of forte non-smokers and smokers who present with lung cancer.
Industrial risks: work and occupations
Asbestos is another risk factor for lung cancer. People who work with asbestos are at increased risk of lung cancer, and if they also smoke, the risk is greatly increased. Although asbestos has been used for many years, Western governments have all but eliminated its use in the workplace and in household products. The asbestos-related type of lung cancer, mesothelioma, often begins in the pleura.
Workers associated with the asbestos, arsenic, sulfur, (the three “A”) industries, vinyl chloride, hematite, radioactive materials, nickel chromates, coal products, mustard gas have an increased risk of developing lung cancer, chloromethyl ethers, gasoline and diesel derivatives, iron, beryllium, etc. Even the non-smoking worker in these industries has a five times greater risk of contracting lung cancer than those not associated with them. All types of radiation are carcinogenic. Uranium is weakly radioactive, but lung cancer is four times more common among non-smoking uranium miners than in the general population, and ten times more common among smoking miners. Radon is a radioactive gas that is produced by the natural disintegration of uranium. Radon is invisible and has no taste or odor. This gas can concentrate inside homes and become a potential cancer risk.
Urban and air pollution
It is conceivable that air pollutants, especially urban ones, play some role in the increased incidence of bronchogenic carcinoma today. Lung cancer is more frequent in the city than in the countryside, due to:
- Humos of explosion engines (cars and motor vehicles in general) and heating systems — sulphur dioxide is one of the most important carcinogenic reducing substances.
- Ground particles of the pavement of the streets.
- Radioactive particles.
- Natural radon gas and radioactivity are very abundant in some geographical areas.
Although most authors acknowledge the existence of a small urban factor in the incidence of lung cancer, the main culprit, by overwhelming numerical difference, is smoking.
Cicatrization: previous bronchial pathology
Certain peripheral forms of lung cancer result from lung scarring. In more than half of the cases, these scar-associated carcinomas are adenocarcinomas and the pathogenic interpretation assumes that malignancy is due to the atypical proliferation of malignant cells in the epithelial regeneration process of these lesions. or that carcinogenic substances, such as cholesterol in old tubercular lesions, have been trapped in the scar tissue. The hypothesis about this fact assumes that this entrapment could be explained by the lymphatic blockage caused by the scar, with the accumulation of histiocytes loaded with viral particles or chemical substances. Some scarring diseases potentially associated with lung cancer include:
- Chronic bronchitis: intimately associated with smokers and increased risk of contracting lung cancer.
- Tuberculosis: It is a chronic irritation of the lung parenchyma that leaves a tuberculosis scar that favors the appearance of lung cancer (carcinoma or scar cancer, especially adenocarcinoma).
- Bronchiectasis, lung infarction zones, inclusions of foreign bodies, idiopathic pulmonary fibrosis (10% die from bronchogenic cancer), sclerodermy and other scars.
Viruses
Certain viruses are known to cause lung cancer in animals, and recent evidence suggests they have a similar potential in humans. The relationship of viruses with lung cancer has two different bases:
- In the experimental field, an incidence of bronchial epithelium metaplasia is assumed by paramixovirus, the human papilloma virus, the papovirus SV-40, the BK virus, JC virus and cytomegalovirus.
- As for human pathology, there is a link with bronchioalveolar carcinoma, probably due to cell cycle alteration and apoptosis inhibition, allowing uncontrolled cell division.
Diet
Some studies conclude that a diet with few plant foods could increase the risk of lung cancer in people who are exposed to tobacco smoke. Apples, onions, and other fruits and plant foods may contain substances that offer some protection against lung cancer.
Certain vitamins, especially vitamins A and C, are thought to be protective of the bronchial mucosa, due to their ability to inactivate carcinogenic free radicals, or due to their ability to precisely regulate certain cellular functions, through different mechanisms. However, there are no studies that have been able to demonstrate that prolonged use of multivitamins reduces the risk of developing lung cancer. Research related to vitamin E shows conclusive evidence that this vitamin, taken in large doses, can increase the risk of lung cancer, an especially important risk among smokers.
Beta-carotene has been shown to be ineffective as a chemoprevention of lung cancer, moreover, since 2007 the use of β-carotene as a chemopreventive supplement for lung cancer is not recommended in individuals with a history of consumption of cigarettes greater than 20 pack-years or with a family or personal history of lung cancer. Studies speculate that beta-carotene, traditionally considered an antioxidant, may be metabolized to "pro- oxidizing" once inside the human organism.
Pathology
Location of lung cancer
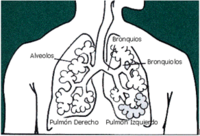
From a topographic point of view, the location predominates in the right lung (ratio 6:4), in the upper lobes and, within these, the anterior segment. Secondly it is located in the lower lobes and thirdly in the median lobe and lingula. Pancoast tumor is the malignant tumor located in the lung apex, which appears in 4% of cases and is not a histopathological variety. Depending on the location, lung cancer is classified as:
- Central lung cancer: appears at the level of major bronchus, parrots and segmentaries (first, second and third generation respectively), up to the fourth generation, i.e. preferably in and around the pulmonary hill. Tracheal origin is rare, about 1 %. It starts with bronchial symptomatology and are accessible with the bronchoscope. They represent 75% of the cases. The epidermoid varieties (squamous cells) and the indifferentiated carcinoma of small cells are central cancers.
- Peripheral lung cancer: appears from the fifth generation bronchus. It starts with extrabronchial clinic and is not accessible with the bronchoscope. Adenocarcinoma is an example, which is usually located in very remote areas, next to pleura.
Macroscopic aspect
In its development, lung carcinoma begins as an area of cytologic atypia in situ, which over an unknown period of time produces a zone of thickening of the bronchial mucosa. From here you can follow one of several patterns:
- Tumor Ulceration of the mucosa: the small focus, usually less than 1 cm in diameter, when progressing acquires the appearance of a verrucous excrecy that elevates and erodes the epithelial lining. It has mamelon edges of irregular contour.
- Intrabronchial tumor: forms a prominence that occupies most of the light of the bronchus.
- Stenosant circular infiltration: predominantly submucosal growth, although it usually ends up ulcerating.
- Peribronchial infiltration: the tumor quickly penetrates the bronchial wall and infiltrates the peribronchial tissue into the carina or mediastinum.
- Invasion of the parenchyma: from one of the above forms, it can reach considerable sizes according to the time elapsed until the diagnosis is made, constituting a solid mass, of firm to hard consistency, of grayish colour or whitish to the court, with some yellowish areas and hemorrhagic foci. The tumor grows on a wide front producing an intraparenquimatous mass in the form of cauliflower that moves the adjacent lung tissue.
- La tumor necrosis is frequent in the epidermoid variety, with formation of a central cavity that ends up infecting many times. This necrosis is an expression of lack of vascularization of the tumor, which is done through the bronchial vessels, and which barely allows the blood supply of the central areas.
- Areas of bleeding: They are often associated with tumor necrosis areas, especially when the tumor is prominent, leading to a white yellow moteado and reblation.
- Secondary injuries: Other associated lesions are distal atelectasis, pneumonic infection also distal to bronchial obstruction caused by the tumor and regional bronchectosis.
Extent or growth of lung cancer
At diagnosis less than 20% have localized spread, 25% have spread to lymph nodes, and 55% have distant metastases. Lung cancer begins at a certain point in the mucosa and from there it has growth towards the interior and exterior of the bronchial lumen, ascending and descending through the submucosa and circumferential growth, following a pattern of direct spread called " infiltration".
- Submucosal growth: can cover the entire bronchial circumference and exceed macroscopic limits. Increasing submucosal growth, cancer will be more unresectable. If an inch beyond the macroscopic limit cannot be removed, the tumor will be irresectable. In its growth the tumor infiltrates the bronchial wall, affecting the submucosal lymphatic plexus, and then spreading through the pulmonary parenchyma according to the interstitial planes, including the perivascular connective tissue of the lung vessels.
- The intrabronquial growth will be responsible for bronchial symptomatology such as cough, hemoptisis, emphysema, atelectasia, etc.
- The extrabronchial growth will be responsible for intratoric extrapulmonary symptoms, derived from the invasion of structures such as mediastinum, chest wall, diaphragm, venas cavas, pericardio, Pancoast tumor, etc. The visceral pleura, which initially resists the spread, ends up being invaded, then infiltrating various intratoraic structures (nerves, pericardium, etc.) or spreading through the pulmonary surface (transpleural implantations) or to the parietal pleura, which if it is invaded also, will quickly be complicated by the progression of the tumor by the torachic wall, with bone structures. In this type of invasion, there is first formation of pleural adhesions, later spreading neoplastic cells through the neoformated lymph vessels from the subpleural lymphatic plexo. This lymphatic involvement is very important and early in lung vertex tumors, in connection with the perineural lymph system of the brachyal plexus, which will have an important clinical translation.
Intra and extrabronchial growth is constant in all lung cancer. Only 20% of the cases, the cancer will be diagnosed in the lung parenchyma (localized), and it is the one with the best prognosis.
Metastasis
25% of diagnosed cases of lung cancer already have affected regional lymph nodes. Even in early stages, about 30% of patients with stage I non-small cell lung cancer die after complete resection of the tumor, due to the presence of undetectable metastases at diagnosis.
Lymphatic dissemination
The frequency of lymph node involvement varies slightly depending on the histologic pattern, but is around 50%. Taking into account the direct continuity of the paratracheal nodes with the supraclavicular nodes, it can be established that all cancers of the right lung and those located in the left lower lobe may invade the nodes of the right supraclavicular fossa, through the great lymphatic vein; On the other hand, the left supraclavicular lymph nodes will be affected exclusively in tumors of the left upper lobe, through the thoracic duct.
- Anatomical bases of lymphatic drainage:
- Pulmonary lymphatics: The subpleural lymphatic network and the lobar and interlobar nodes are included here; of these, it is particularly important to those located between the mid lobar bronchus (right lung), or segmentaries of the lyngual (left lung), and the apical segment bronchus of the lower lobe (sect. 6), since by its interlinphatic connections drained the same lymphb. The hilar nodes represent the limit between this lung group and extrapulmonary.
- Extrapulmonary Ganglios: are the subcarinal nodes, located under the tracheal fork, and the paratracheal nodes. The previous and paraesophageal mediastinal nodes already represent distant ganglionar stations.
- Extratoric Ganglios: the most important groups are supraclavicular, abdominal paraaortics, cervical and axillary.
- Lung lymphatic territories:
- Superior: includes the upper lobe, with the exception of the posterior and lateral portions on the right side, and the lingular portion and part of the previous segment on the left. The lymphatic drainage is made towards the paratracheal nodes and then the ipsilateral supraclavicular nodes (on the left side there is also an important pathway of propagation to the previous mediastinal nodes).
- Media: with the previously excluded portions of the upper lobes and the medium lobe and the segment 6 from the lower left lobe. The lymphatic drainage is made preferably to the subcarinal nodes, and of these, to the paratracheals of the corresponding side, although sometimes only to the paratracheal rights.
- Inferior: represented by the entire lower lobe, except the mentioned apical or segment 6. Lymph drainage is done to the paratracheal subcarinal nodes. Tumors in this lower territory often affect the nodes located in the lung ligament (functionally, these have the same physiological meaning as the hilarious nodes), from which they progress to subcarinal nodes or, more rarely, to paraesophageals.
- Carcinomatous lymphangitis: it is a very peculiar anatomopathological picture, characterized by presenting a wide area of the lung an edematous and atelectassic aspect, with infiltration reggae that radiately extend from the hiliar region to the peripheral subpleural lymphoma. Considered some years ago of a metastatic nature, it is actually a diffuse infiltration in centrifugal sense from the hilar ganglias blocked by the proliferation of neoplastic cells to the subpleural plexo.
Bloody spread (distant metastasis)
40% of non-small cell carcinomas and 70% of small cell carcinomas already have distant metastases at the time of diagnosis. Distant metastases are frequent, a fact that is justified by the relatively small involvement early pulmonary venous vessels; In the histopathological variety of anaplastic cell tumors in oat grains, it is almost systematic, which has a very poor prognostic significance. Metastases preferentially affect, and in decreasing order, the liver (30-50%), brain (20%), skeleton (20%), and kidney, with a high incidence in the adrenal glands, which is observed in about 30 -50% of autopsies of patients who died from lung cancer. Perhaps it is the result of distant lymphatic dissemination by connection of the para-aortic nodes with other retroperitoneal groups, and not by hematogenous route. Finally, we must also mention metastases in the lung itself, as a result of an embolization through the pulmonary artery. However, the existence of several tumor masses, unilateral or bilateral, also leads us to consider that they are bronchogenic disseminations, as is admitted in bronchoalveolar tumors.
Diagnosis
In most patients, the diagnosis is made based on clinical data and when a radiological study detects a lung abnormality. Less frequently, an attempt will be made to specify the diagnosis in patients in whom a suspicious image has been revealed in a routine radiological study or an attempt is made to locate the tumor based on a histological study that shows neoplastic cells.
General complementary tests
Supplementary tests are usually performed on patients with lung cancer to determine the patient's general condition, including a complete medical history and physical examination, complete blood count, blood biochemistry (electrolytes, serum glucose, calcium, and phosphorus, and liver function and renal, albumin and LDH), electrocardiogram, pulmonary function tests such as spirometry and arterial blood gases, coagulation tests, tumor markers such as carcinoembryonic antigen (CEA) and alpha-fetoprotein (AFP).
Plain chest X-ray
Simple chest radiographs can show some abnormality in almost 98% of patients with bronchogenic carcinoma, and 85% are suggestive images to suspect the diagnosis due to distal lung changes (atelectasis), the existence of lymphadenopathy (mediastinal widening) or detection of chest wall invasion. Chest radiography detects suspicious elements in most patients with lung tumors. Serial x-rays are not recommended for early detection of lung cancer.
Computerized axial tomography
Computed axial tomography is very useful in lung cancer and is recommended in all patients with a solitary pulmonary nodule detected by radiography. Some advantages of a CT scan include:
- It finds its main application in the determination of the extent of neoplasia; both intrathoracic and extrathoracic, and of mediastinal adenopathies.
- In the differentiation between benign and malignant nodules, in addition to the detection of small nodules with greater clarity than in simple x-rays. They provide valuable information on the existence of cavitation, calcification and at times the intrabronchial location of the tumor, finally, of the morphological characteristics of the tumor.
Archiduque Luis Salvador de Austria
El archiduque Luis Salvador de Austria (en catalán: Arxiduc Lluís Salvador) fue el artífice del turismo en las Illes Balears. Llegó por primera vez a la isla en 1867, viajando bajo su título de "Conde de Neuendorf". Más tarde se instaló en Mallorca, comprando terrenos agrestes para conservarlos y disfrutarlos. Hoy en día, varias rutas de senderismo llevan su nombre.
Con el broncoscopio rígido se puede explorar un amplio territorio bronquial que comprende tráquea, bronquios principales y bronquios lobares inferiores en visión directa. Por medio de ópticas es posible llegar a visualizar la salida de los bronquios lobares superiores. Su limitación viene dada por la imposibilidad de introducirse en bronquios segmentarios y obtener muestras de lesiones periféricas. Por el contrario, el broncofibroscopio consigue una visualización prácticamente total del árbol bronquial, llegando a territorios realmente periféricos, obteniéndose, sin duda, un aumento considerable de la rentabilidad. La broncoscopia rígida apenas se utiliza quedando completamente desplazada por la fibrobroncoscopia.
Bronchoscopy allows direct visualization of the tumor, since most of these are central and accessible with this exploratory technique.
Cytology
Sputum cytology is the most common diagnostic procedure in patients with suspected lung cancer and should be the first technique to be used in all patients suspected of suffering from lung cancer, either because it is suggested by the clinic and radiology, either because, even if they are not suggestive, it is a high-risk individual. As of 2007, individual or serial sputum cytology is not recommended for lung cancer screening.
Fine needle aspiration (FNA) is especially useful in the diagnosis of bronchogenic carcinoma. It has a sensitivity of 80%, which improves in certain thoracic locations to 100% guided by endoscopic ultrasound. It is only indicated in peripheral tumors not accessible to fiberoptic bronchoscopy or in medium-sized tumors in which it has repeatedly failed to obtain Inflammatory or necrotic material. In masses of 3-4 cm in diameter or larger, a yield of around 80% is achieved, but it manages to obtain material from lesions as small as nodules of 1 cm in diameter.
Biopsy
Biopsy provides maximum certainty in the diagnosis of lung cancer. There are different modalities depending on the clinical circumstances, the main one being bronchial or transbronchial biopsy in the course of fiberoptic bronchoscopy. Percutaneous, transparietal, or transpleural lung biopsy is generally performed under radiological control using various methods such as aspiration biopsy, sharp needle biopsy, and ultra-rapid compressed-air drill.
The main indication is in those peripheral tumors that are difficult or impossible to access by other procedures. If the tumor is peripheral and there is pleural effusion, a pleural biopsy can be used. It can be done with different types of needle, the most used being the Vim-Silverman. If metastasis is suspected, lymph node biopsy obtained by mediastinoscopy or percutaneous biopsy of palpable lymph nodes is indicated. Other types of biopsy, including bone or bone marrow biopsy, may be helpful in some patients.
Mediastinoscopy
Mediastinoscopy is aimed at visualizing the anterior mediastinum, usually to remove tissue (biopsy) from a lymph node surrounding the airways or any unusual tumors. A small incision is made at the base of the neck and a device called a mediastinoscope is inserted up to the middle part of the thorax, being able to reach the pulmonary hilum. Despite being an invasive technique, different studies have shown its effectiveness. efficacy in the preoperative staging of lung cancer and in the diagnosis of mediastinal lesions.
Other studies
The use of radioactive isotopes, mainly macroaggregates of albumin labeled with I131 or Technetium 99 for the study of pulmonary perfusion. Gallium 67 scintigraphy is also available for the detection of metastases, especially lymph nodes. It is carried out with bleomycin labeled with Co57 or with Ga67. Another technique that is used is Positron Emission Tomography (PET) that uses glucose labeled with a radioactive atom.
Intrathoracic and extrathoracic extension studies use different exploratory methodologies and with various purposes, including knowing the extension of the tumor or metastases.
Determination of staging
For many reasons, including comparing treatment outcomes, the existence of a uniform TNM method for staging cancer based on its anatomical extent at diagnosis is helpful.
| Stage | Criteria | |
|---|---|---|
| Hidden carcinoma | TX, N0, M0 | |
| Stadium 0 | TIS, Carcinoma in situ | |
| Stadium I | IA | T1, N0, M0 |
| IB | T2, N0, M0 | |
| Stadium II | IIA | T1, N1, M0 |
| IIB | T2, N1, M0 or T3, N0, M0 | |
| Stadium III | IIIA | T3 (or T1 or T2 with N2), N0, N1 or N2, M0 |
| IIIB | Any T, N3 (or any N with T4), M0 | |
| Stadium IV | Any T, any N or M1 | |
Primary tumor (T):
- T0 - No sign of a primary tumor.
- TX - Occult cancer, shown in bronchial washing cytology, but not radiologically or in fibrobronchoscopy. Broncopulmonary secretions contain malignant cells, but there are no other data on the existence of lung cancer.
- TIS - Carcinoma in situ
- T1 - Less or equal to 3 cm in larger diameter, surrounded by visceral pulmonary or pleural tissue and without proximal invasion of the lobar bronchus in fibrobronchoscopy. In addition, rare, superficial, tumors of any size are classified into T1 with limited invasion of the bronchial wall that extend proximally to the main bronchus.
- T2 - Tumor greater than 3 centimeters in larger diameter or tumor of any size that invades visceral pleura or with obstructive atelectasia or pneumonitis that extends to the boiling region. In bronchoscopy, the proximal extension of the tumor may be limited to the lobar bronchus or at least 2 cm of the carine. Atelectasis or obstructive pneumonitis should not affect a whole lung.
- T3 - Tumor of any size with direct extension to the rib wall (including the tumors of the upper cissure) diaphragm, mediastinal or pericardial pleura, without heart involvement, large vessels, trachea, esophagus, vertebral bodies or a tumor of the main bronchus less than 2 cm of the carine, without infiltration of the same. Atelectasis affects a whole lung. There is non-evil pleural effusion.
- T4 - Tumor of any size with infiltration of the mediastinum or heart, large vessels, trachea, esophagus, vertebral or carine bodies or with malignant pleural effusion. Non-hematic or exudative pleural effusions and with several negative cytological studies are not classified as malignant for the purpose of determining the stadium.
Regional lymph nodes (N):
- N0 - No demonstrable metastases in lymph nodes
- N1 - Metastasis in the peribronchial lymph nodes or ipsolateral iliars, or both, including the direct extension of the tumor.
- N2 - Metastasis in ipsolateral mediastinal or subcarinic nodes.
- N3 - Metastasis in the mediastinal or contralateral, ipso or contralateral or supraclavicular nodes.
Distant metastasis (M):
- M0 - No known distant metastases.
- M1 - Remote metastases present, specifying their location for example in brain.
The International Association for the Study of Lung Cancer classifies small cell lung cancer into only two stages: disease localized to the thorax and disease spread outside the thorax.
Lung cancer treatment
Treatment options for lung cancer are surgery, radiation therapy, and chemotherapy, alone or in combination, depending on the stage of the cancer, the cell type of the cancer and how far it has spread, as well as the patient's health status. For this reason, it is very important that all necessary diagnostic tests are performed to determine the status of the cancer.
Surgery
If diagnostic investigations confirm the presence of lung cancer, a CT scan can determine whether the disease is localized and surgical approach is possible, or whether the spread is such that it cannot be cured with surgery. Blood and lung function tests are also expected to be done to determine if the patient is fit for surgery and if there will be enough healthy lung tissue left after surgery. If poor respiratory reserve is discovered, such as in smokers with chronic obstructive pulmonary disease, surgery may be contraindicated. Some advances in surgical techniques have made surgery possible in patients with serious coexisting medical problems.
Some surgical procedures include:
- If a lobe is removed from the lung, the procedure is called lobectomy.
- If the entire lung is removed, the surgery is called pneumocectomy.
- Removal of part of a lobe is known as segmentectomy or resection in wedge.
In those patients with adequate respiratory reserve, lobectomy is the preferred approach because it minimizes the likelihood of localized recurrence. If the patient's lung functions are poor, a wedge resection is advised. Possible complications include significant bleeding, wound infection, and pneumonia. Because the surgeon must cut through the ribs to reach the lung, the ribs will hurt for a while after surgery. Activities are limited for at least one to two months.
Lung surgery has a near post-operative death rate of 4.4%, depending on lung function and other risk factors.
Criteria of irresibility
The possibility of surgical removal of all tumor tissue is understood to be resectable. The presentation of extrapulmonary intrathoracic tumors are absolute surgical contraindication because they are irresectable. The function of the criteria of irresicability is to specify surgical contraindications, operating only to the patients who can be completely dried from the tumor, avoiding useless thoracotomies. Some criteria that make lung cancer unresectable include:
- Distance metastases: is included in this concept, in addition to the involvement of different organs and structures, either more than one at a time or a single organ with diffuse tumor extension (hyde, bone, brain, adrenals, skin, etc.), the infiltration of the supraclavicular pre-scalénic fat (the adhesive tissue located in the depth of the supraclavicular region, in front of the escalenal muscles), the involvement of another
- Upper or lower vena cava syndromeeither by infiltration or compression or both at once. Here radiation therapy has an urgent indication.
- Commitment of both liver lobes.
- Extensive affect of the chest wall or pleural spillcontaining neoplastic cells (discovered by cytology or positive biopsy), metastatic or hemorrhagic.
- Any stadium T4. They usually have a yield scale of Karnofsky less than 50%, indicating that their ability to perform reduced tasks is reduced to 50%.
Inoperability criteria
They are established according to the clinical-functional situation of the patient: the situation in which it is before the intervention, and the possibility of functionally supporting the degree of lung resection that is required in each case.
- According to the general characteristics of the subject:
- Advanced chronological age. It is normally established in persons over 75-80 years of age.
- Important cardiovascular disease: recent acute myocardial infarction (with less than 3-6 months of evolution), arrhythmias, malignant hypertension, refractory heart failure, acute stroke.
- Non-controllable associated severe disease: coagulopathies, kidney failure in hemodialysis, cirrhosis, evolved diabetes.
- Malnutrition.
- According to the respiratory function:
- Preoperative VEMS less than 1 L, or less than 50% of the theorist. With VEMS between 1 and 2 liters it will improve with bronchodilators and quit smoking. With FEV1 or VEMS/2003/2 L there is no problem.
- Postoperative VEMS calculated less than 8 dL; Resection would prevent the patient from carrying a normal physical activity, because it would have resting dyspnea.
- Life capacity less than 45-50 %.
- Dissemination less than 50%.
- Patient with emphysema, chronic bronchitis, with obstructive, restrictive or mixed radiological pattern and diminished functional capacity.
- Respiratory insufficiency: pO2 vis60 mmHg and pCO2/2005 45 mmHg.
On the one hand, a functional study with xenon should be performed by measuring the percentages of ventilation and perfusion in each lung separately and even right catheterism. On the other hand, an assessment of the possibility of intervention based on these data and the resection to be performed to remove the tumor.
Radiation therapy
Radiation therapy involves the use of ionizing radiation, such as high-energy X-rays, to destroy cancer cells and shrink tumors.
External radiation therapy uses radiation therapy that is generated outside the body by a linear accelerator and is focused on the cancer. This type of radiotherapy is the most frequently used to treat primary lung cancer or its metastases in other organs.
In internal radiotherapy or brachytherapy, small pills of radioactive material or isotope are used that are placed directly in the cancerous area or in the airway near the cancerous area. This type of brachytherapy is generally palliative and its main indication It is an obstructive atelectasis due to cancer. Brachytherapy at the resection margins may reduce recurrence.
Radiation therapy is sometimes used as the main treatment for lung cancer, especially when the patient's general health is too poor for surgery. It can also be used to help relieve blockage of the great airways airways caused by cancer.
Radiation therapy may be used after surgery to destroy very small remnants of cancer that cannot be seen or removed during surgery (residual microscopic disease). Additionally, radiation therapy can be used to relieve some symptoms of lung cancer such as pain, bleeding, difficulty swallowing, and problems caused by brain metastases.
Side effects of radiation therapy can include mild skin problems, nausea, vomiting, and tiredness. Often these side effects last for a short time. Radiation therapy can also worsen the effects of chemotherapy. Radiation therapy to the chest can damage the lungs and cause difficulty breathing. The esophagus is in the center of the chest and will be exposed to radiation therapy. For this reason, difficulty swallowing may be experienced during treatment (oesophagitis). These effects will improve after the end of treatment.
Chemotherapy
Chemotherapy involves the administration of antineoplastic or cytostatic drugs intravenously or orally to prevent the multiplication of cancer cells. These drugs enter the bloodstream and reach all areas of the body, allowing the cancer to spread. treatment is useful even for those cancers that have spread or metastasized to organs distant from the lung. Depending on the type and stage of lung cancer, chemotherapy may be given as the main treatment (primary) or as an adjunctive treatment (adjuvant) to surgery or radiation therapy. Chemotherapy for lung cancer usually uses a combination of anticancer drugs (polychemotherapy).
Cisplatin (CDDP), or its similar, carboplatin, are the most commonly used chemotherapeutic agents to treat non-small cell lung cancer (NSCLC). Recent studies have found that the combination of either of these with drugs such as gemcitabine, paclitaxel, docetaxel, etoposide (VP-16), or vinorelbine appear to improve efficacy in the treatment of NSCLC. Gemcitabine was initially approved for the treatment of pancreatic cancer and is now widely used in the treatment of NSCLC. Vinorelbine is an alkaloid that inhibits mitosis in cells in the M phase of the cell cycle by inhibiting tubulin polymerization. Myelosuppression, i.e., a reduction in the production of granulocytic lineage of blood cells whites is the only dosing-limiting adverse effect of these drugs. Clinical trials continue to investigate the best way to use this drug combination. Other drugs Some have appeared with promising results, such as pemetrexed, recommended for locally advanced and even metastatic stages of NSCLC.
Some of the usual combinations of chemotherapy drugs used for patients with small cell lung cancer (SCLC) include:
- EP (etoposed and cisplatin)
- ET (data and carboplatin)
- ICE (ifosfamide, carboplatin and etoposide)
- CAV (cyclophosfamide, doxorubicin or adriamicin and vincristine).
Newer drugs such as gemcitabine, paclitaxel, vinorelbine, topotecan, and teniposide have shown promising results in some SCLC studies. If the patient's health is relatively good, higher doses of chemotherapy may be given along with drugs called growth factors (neutrophil or macrophage colony-stimulating factor and erythropoietin). These help prevent the side effects of chemotherapy on the bone marrow.
Chemotherapy drugs kill cancer cells, but they also damage some normal cells. The side effects of chemotherapy depend on the type of drugs used, the amount given, and the length of treatment. Temporary side effects may include nausea and vomiting, loss of appetite (anorexia), hair loss (alopecia), and mouth sores (mucositis). Since cisplatin, vinorelbine, docetaxel, or paclitaxel can damage nerves, numbness may be experienced, particularly in the fingers and toes, and sometimes weakness in the arms and legs (neuropathy).
Some studies have suggested that marijuana-derived cannabinoids used during chemotherapy have reduced nausea and vomiting associated with treatment, allowing the patient to eat.
Therapy
Recently, biological therapy or immunotherapy has been approved in some countries for the treatment of lung cancer. Immunotherapy may be indicated in conjunction with surgery, chemotherapy, and radiotherapy. These biologic therapies use the body's immune system, either directly or indirectly, to fight the cancer or to lessen the side effects that some cancer treatments can cause. The compounds approved for lung cancer are EGFR tyrosine kinase inhibitors (epidermal growth factor receptor) such as erlotinib and gefitinib (in patients with EGFR mutated only); monoclonal antibodies such as cetuximab (directed against EGFR) or bevacizumab (directed against vascular entoryl growth factor receptor or VEGFR) in combination with chemotherapy; and crizotinib in patients with translation of the EML4-ALK genes. In Argentina and Cuba, racotumumab is approved, a monoclonal antibody that induces an immune response against NGc gangliosides present in tumor cells.
The progress that has been made in understanding the biology and oncogenetic mechanisms of lung cancer has enabled the development of treatments based on the molecular composition of cancer cells. Some of the molecular targets studied include vascular growth factor and its receptors, as well as the epidermal growth factor receptor. These drugs appear to be safer and more effective in certain histological subtypes of lung cancer, particularly non-cell lung cancer. -small and its advanced stages. The only disadvantage so far is that a histological diagnosis of the cancer is required.
Lung cancer prevention
Primary prevention through cessation or avoidance of tobacco use, along with early detection represent the most important lung cancer control measures. Anti-smoking efforts beginning since the 1970s have resulted in a stabilization of the death rate from lung cancer in white men, while among women the cases are still increasing, since this group has increased the prevalence of consumption, decreased the age of onset and increased the number of cigarettes smoked. Not all cases of lung cancer are due to cigarette smoking, as the role of passive smoking has been increasing in importance as a risk factor for lung cancer. This has encouraged the creation of policies to reduce the risk of lung cancer. contact with cigarette smoke among non-smokers.
Smoke from automobiles, industry, and power plants also pose a risk of lung cancer. Multivitamins taken long-term do not help prevent lung cancer, while vitamin E appears to increase the risk of lung cancer in smokers.
Secondary prevention
To prevent lung cancer from reaching clinical manifestations, health policies focus on diagnosis or early detection of the disease through screening and tumor control programs. Another way of carrying out secondary prevention is by making the population aware through publicity campaigns of the initial symptoms of suspected lung cancer. Screening with chest X-ray or sputum cytology in asymptomatic people is not recommended.
Early detection of lung cancer through screening is unlikely to reduce mortality rates, although it has been shown to improve survival of patients diagnosed with the disease.
Contenido relacionado
Spirometer
Hematopoiesis
Joseph Bell