Huntington's disease
Huntington's disease (HD), also known as Huntington's chorea, is a serious and rare hereditary neurological degenerative disease. HD is named in honor of George Huntington, an American physician who described the disease in 1872. He was the first person to identify the hereditary nature of HD.
Development of the disease can follow very different paths, even among siblings and close relatives. This is because, together with the specific mutation of the huntingtin protein, other hereditary factors are also involved.
The disease causes psychiatric and motor impairment, with very slow progression, over a period of 15 to 20 years. The external feature most associated with the disease is the exaggerated movement of the extremities (choreic movements) and the appearance of sudden grimaces. In addition, it becomes progressively difficult to speak and remember. In the final stages of the disease, the duration of the movements is lengthened, keeping the limbs in complicated and painful positions for a time that can last up to hours.
However, severe mental disorders, which normally precede muscular ones, are the characteristic features of the disease. This can trigger repeated depressive episodes with negative repercussions in the environment of relatives. Cognitive faculties decrease, as well as memory, and the ability to concentrate worsens. The disease ends up being the cause of dementia in patients. Also, it should be said that the suffering caused by the disease itself and its sequelae can lead to a desire for suicide.
In 1872, the physician George Huntington first observed this disease in an American family of English descent and gave it the name "Huntington's disease." The alternative name of "chorea" comes because among its visible symptoms we find choreic movements, that is, involuntary and sudden movements of the extremities. It is believed that its origins must have been in northwestern Europe and that from there it spread to the rest of the world, especially to America where we find high rates of this condition. In 1933 it was discovered that the trigger for the disease was a genetic mutation located later on chromosome 4, which was published in the journal Nature in 1982 by the genetics team at the Faculty of Medicine in Harvard University, Boston.
The largest known population with Huntington's disease is found in the region of the western coast of Lake Maracaibo (Zulia State, Venezuela), and it is estimated that it arrived there at the beginning of the 19th century and that, as a consequence of a founder effect has been maintained and there are many members of the population who suffer from it and those who do not have a high risk of suffering from it. Thanks to this population, and to the samples for analysis provided by its members, in 1983, various research teams, including J.F. Gusella, discovered through linkage techniques the exact location of this disease in the human genome. The responsible gene is the so-called "huntingtin gene" that we find near the telomere of the short arm of chromosome 4.
It is estimated (2006) that there are around 45,000 people affected throughout Europe. In North America, about 30,000.
After reaching the age of majority, any individual can have a predictive exam and thus obtain the certainty or not of their presence years and even decades before their first symptoms. The genetic test is infallible, since all carriers of this genetic mutation will sooner or later become a victim of the disease.
Currently, there is also preimplantation diagnosis: in vitro fertilization, it is analyzed which of the embryos that have begun to develop have the disease, and which do not, implanting only the healthy one, in such a way that the desired child does not will be affected by this disease.
Etiology
The disease is caused by a single hereditary factor. The genetic defect is found at the level of chromosome 4. It affects a protein of unknown function and expression in numerous tissues, called Huntingtin. The defect is due to an expansion of CAG triplets that code for glutamine synthesis. In the original sequence there are 34 repeats, and in the disease, more than 40. Although the pathophysiological bases of the disease are not yet fully established, it is believed that these "additional glutamine tails" cause the proteins to interact with each other in a unique way. hydrophobic and facilitates the formation of protein precipitates and accumulations, especially in the brain.
The number of recurrences is related in direct proportion to the severity of the symptoms and is inversely proportional to the age of presentation. In this type of diseases due to triplet expansion, it is common that a slight increase in the number of repeats does not produce the disease, but that this increase is transmitted to future generations, producing, in each gametogenesis, an increase in the number of repeats., until finally inducing the disease. By the time it is established, inheritance is autosomal dominant (meaning each offspring has a 50% chance of inheriting the disease).
One of the characteristics of this type of triplet expansion disease is gene anticipation, that is, as the generations go by, the number of repeats increases, and this makes the disease manifest earlier and more aggressively in future generations. In addition to the phenomenon of gene anticipation, the phenomenon of genetic imprinting is also common in this type of disease. In the case of Huntington's disease, genetic imprinting is paternal, which means that changes in huntingtin gene expression occur through the paternal germ line (in terms of genetic condition, the elongation of the region where the trinucleotide repeats are located occurs in paternal meiosis, in the formation of gametes).
Juvenile Huntington's Disease
Juvenile Huntington's disease (JHD) is a form of Huntington's disease (HD) characterized by the onset of signs and symptoms before the age of 20. The exact prevalence of the juvenile form is unknown, but is estimated to be around 1/166,000.JEH has been described in 6% of all HD cases, with a prevalence of 1/10,000.
Behavioral disturbances and learning difficulties at school are often the first signs. The motor disorder is often hypokinetic and bradykinetic with dystonic components. Dementia is present in early stages of the disease. Chorea, the classic sign of HD, is rarely seen in the 1st decade and only appears in the 2nd decade. Seizures, ataxia, and weight loss are common.
HD is caused by an expansion of the CAG triplet repeats (36 repeats or more) on the short arm of chromosome 4 (4p16.3) in the huntingtin gene, HTT. In juvenile Huntington's disease, the CAG repeat length is greater than 55 in most cases. The length of the expansion determines about 70% of the variation in the age of onset of symptoms, but it does not offer information about the initial symptoms, their course, or the duration of the disease. In 75% of patients with JEH, the father is the affected parent.
Diagnosis is based on compatible clinical manifestations in an individual with a parent with proven HD, and is confirmed by DNA testing. Presymptomatic diagnosis has been codified in the guidelines of the International Huntington Association (IHA) and the World Federation of Neurology (WFN) Research Group, and it is not performed in at-risk patients under 18 years of age. Differential diagnoses of JEH include: juvenile-onset spinocerebellar ataxia (SCA) type 2 (SCA2: 12q) with chorea, dystonia, and dementia; dentato-rubro-pallido-louisiana atrophy (DRPLA: 12p) with chorea and myoclonic epilepsy; SCA 3 (14q) with rigidity, ataxia and dystonia and SCA17 (6q) with psychiatric disorders and dementia. Other causes of chorea such as systemic diseases or iatrogenic causes should also be considered.
Sydenham's chorea and post-strep chorea are still present in many parts of the world. There is no curative treatment available at present. Its management must be multidisciplinary and is based on symptomatic treatment in order to improve the quality of life. Chorea can be treated with dopamine receptor blockers (risperidone, tiapride, pimozide) or dopamine depleting agents (tetrabenazine). None of these drugs has been officially approved for use in children, but they are prescribed to treat the main symptoms of the disease. Attempts have been made to treat hypokinesia with a number of drugs, but without success. Paramedical care with speech, occupational and physical therapy, and psychological help for the patient and family is also recommended. The progression of the disease entails complete dependence on daily life, resulting in patients requiring full-time care, and ultimately death. The average duration of the disease is similar to or slightly shorter than that of the adult. The most common cause of death is pneumonia.
Incidence and prevalence
It is estimated that the average prevalence is between 5 and 10 affected per 100,000 inhabitants, with a global distribution that is equal between both sexes, while the average annual incidence is 1 to 4 cases per million inhabitants. Despite the fact that the distribution is global, it is known that there are notable differences between human groups, being the populations of East Asia and the black population, for example, less prone. The origin of the disease has been determined, on the basis of genealogical studies, in Europe (mainly France, Germany and the Netherlands), with its spread to America, Africa and Australia being a later process. The highest prevalence is observed today in Lake Maracaibo (Venezuela), on the island of Tasmania and in Moray Fjord (United Kingdom).
Diagnosis
If you think you have HD, you should see a specialist in this disease (usually a neurologist) to perform some diagnostic tests, both clinical and genetic. If you already have symptoms of the ailment, the doctor will diagnose you based on medical history and clinical tests. The results of this diagnosis will be contrasted with the results of the genetic tests (confirmatory tests). If you do not have any symptoms, but are at risk because one of your parents has HD, you may be an asymptomatic carrier of the altered gene. In this case, the diagnosis will be based solely on genetic testing.
The genetic test that is carried out is called a “predictive test”, and it makes it possible to determine if a person will develop a genetic disease. As its name indicates, it is performed on pre-symptomatic people, that is, without signs or symptoms of the disease. Each person must decide if they want to pass the predictive test or not. Some people feel very uncomfortable not knowing if they are carriers of the mutation or not. For others, however, the knowledge that they are about to develop a fatal disease is even worse.
It can be very worrying to live knowing that there is a risk of developing HD; sometimes it is better to know for sure whether or not you have the abnormal gene for the disease. At this point, genetic counseling is highly recommended. Going to a genetic clinic allows you to have accurate and up-to-date information about the disease. It also gives an opportunity to discuss the various options available. Usually a consultation is held with a geneticist, who allows you to discuss all your doubts regarding HD. If you decide to take the predictive test, you will have several medical appointments with the team that will guide you throughout the process. A blood sample would also be drawn. The disclosure of the results would take place at 2-8 weeks, depending on the center where you were treated.
In general, the recommended minimum age to pass the predictive test is 18 years, since it is assumed that the person is mature enough to be aware of what it means to be a carrier of the abnormal gene. In exceptional cases, it may be advisable to carry out the genetic test in children who, for example, show signs of juvenile HD or in children under 18 years of age if they are pregnant.
Genetic testing is only available at specialized genetic clinics. You must request to see them through your GP. DNA is usually extracted from the blood cells of the potential carrier, but sometimes the blood of the parents is also tested to confirm the diagnosis of HD. Genetic analysis is a DNA test that determines the number of CAG repeats of the Huntington gene and thus detects the HD mutation. The test can determine whether or not you carry the mutated gene, but it cannot determine when the disease will develop.
Four types of results can be distinguished:
Below 27 CAG repeats means you're a normal person.
Between 27 and 35 repeats means you're a normal person, but with a small risk of the number increasing in future generations.
Between 36 and 39 repeats, the result is abnormal, but there is a possibility that the disease may develop at a very old age or not at all.
Above 40 repeats, the gene is abnormal.
HD is one of the few inherited diseases for which genetic testing is possible. Normally these tests are confirmed in duplicate with two different blood samples. The results are confidential and are only given to a third party with written permission.
Depending on what stage of the disease you are in and whether your genetic condition affects other people, it can be very important to communicate your situation to those around you. For example, your spouse or partner should know that you carry the gene. If the symptoms of the disease start to affect your work performance, you should inform your bosses. But you have to keep in mind that sometimes informing others involves loss of social contact, as well as discrimination at work and by insurance companies. Before making a decision on this, you should consult a specialist in legal aspects related to HD. Always keep in mind, that HD is deadly in the very long term. The average duration of the disease from the onset of symptoms until death is about 15 to 20 years, so making any type of decision from the moment you know you are a carrier must be made with the greatest guarantees. and certainty that it is what is best for us.
Prenatal test
The mutation responsible for HD is an expanded trinucleotide (CAG) repeat in the huntingtin gene on chromosome 4, predictive presymptomatic and prenatal testing has been possible since 1993 by direct mutation analysis. Using linkage analysis it is also possible to perform exclusion testing so that chromosome 4 at 50% risk can be identified as being present in the fetus or not. This allows a person to have children who have not inherited the disease, even if the parents do not want their own condition to be defined. Using this method means that pregnancies that are not at risk can be terminated.
Some parents want to know the risk to the fetus, but not their own. DNA-linked markers are used, rather than a direct genetic test. The test does not look for the HD gene in the father. Indicates whether the fetus has acquired chromosome 4 from an affected or unaffected grandparent in a family with HD.
If the test shows that the fetus has inherited chromosome 4 from the affected grandparent, the parents know that the risk is the same as the father's (50-50). If the test shows that the fetus has acquired chromosome 4 from an unaffected grandparent, the risk is very low (<1%).
Taking into account the technical feasibility of prenatal testing in HD, and the severity of the disease, it might be expected that prenatal diagnosis is requested frequently. However, many couples express anxiety about having children at all, as they do not want any child of their own to grow up with an affected parent, even though it is known that the child would not be at risk due to prenatal testing.
Tyler examined a group of references to the pregnancy exclusion test in the period 1986-1989. The authors surveyed a group of individuals at 50% risk of developing HD about their attitudes toward prenatal testing. Fifteen of a total of 90 couples referred for exclusion testing underwent testing in 24 pregnancies. They concluded that the demand for these tests is likely to be small. The most common reason for not going ahead with testing is upset about the termination of the pregnancy. The authors stressed the need for intensive counselling, as many couples were uncertain about how the test worked.
In addition, people who used the diagnosis during pregnancy reported less than had been their original intention. Forty-three percent of this Canadian group who entered the presymptomatic predictive testing program reported using prenatal testing. In the study period, 18% of those with unfavorable results, who had had a pregnancy, used prenatal tests. In a survey of people from Germany who were at risk of HD, five more than 67% indicated that they would be willing to undergo presymptomatic predictive testing themselves, but only 45% wish to use prenatal diagnosis. Twenty-seven percent of those surveyed declared that they could not use prenatal diagnosis, since they considered that they could not terminate a pregnancy.
Despite the low use of prenatal testing, data are available from centers of many people who undergo it describing the high-definition presymptomatic prediction tests that family planning gives as one of the main reasons for undergoing to this exam.
Ethical-social implications and genetic counseling
Currently, and more specifically in this disease, its future manifestation can be determined long before the first symptoms begin in a patient and also the risk to which family members are exposed. This determination requires an analysis of DNA markers close to the huntingtin gene, but the samples must also be from members of the patient's family. In addition, it must be added that a presymptomatic diagnosis can translate into a death sentence, since there is no cure for Huntington's disease. All this implies a series of ethical-social problems that physicians and genetic counselors have to take into account.
For example, if it is a presymptomatic test, the patient must give their consent for their relatives to be informed of the result and the consequences that affect them; in the opposite direction of the chain of events, the relatives must agree to transfer their blood samples and each related person must be informed about the consequences that their decision may have and have the full right to make their own decision. In this way, everyone has the right not to know her situation, but this conflicts with the right of family members to know that information. This is a problem with confidentiality (required in medicine) in tests of relatives and in fact, in studies that have been carried out, 50% of the relatives of patients with Huntington's Chorea have refused to know their status with respect to the huntingtin gene.
Clinic
Huntington's disease is characterized by the presence of progressive motor, cognitive, and psychiatric alterations in subjects with a family history compatible with autosomal dominant transmission. The variability of the age of onset is determined in 60% by the number of CAG triplets, while the rest is attributable to other genetic and environmental factors (Wexler 2004). In this way, the subjects with the greatest number of repetitions present an earlier age of onset, existing from juvenile and even infantile forms to forms of presentation in old age. In addition, the number of triplets determines the phenotypic variability of the picture.
Some studies have suggested the existence of three different evolutionary groups based on neuropsychological deterioration:
- Signs of subcortical deterioration: dysarria, bradypsychia, bradiinesia and pseudoalteration of memory. These alterations respond to alterations of the basal nodes of the early states of the disease.
- Signs of subcortical impairment plus signs of frontal dysfunction: alterations of mental and written computation, verbal adinamia, certain degree of agraphy, alterations of motor sequencing and inhibition capacity.
- Aphaso-apraxo-agnosic signs and a greater involvement of motor and premotor functions, which could reflect a generalization of degeneration that would affect the cerebral cortex, proper to the advanced stages of the disease.
As the disease progresses, the deterioration of intellectual functions becomes more evident, especially the manipulative factor, and interquotient differences between the verbal and manipulative factors are observed. A decline in intelligence quotient (IQ) is seen, although an IQ < 70 in subjects with less than 10 years of evolution. However, the overall IQ is usually < 100.
Linguistic functions are preserved in early stages of the disease.
- In initial phases, neurodegeneration affects the anteromedial zones of the captive and dorsal of the whoremen. The first has connections with the front dorsolateral cortex. The second receives references from the premotor cortex. Joint alterations are detected (hypercintic artery). Spontaneous language is observed: few linguistic errors, few semantic paraphasias, few paragramatic or agrarian errors, preserved repetition, a preservation of the denomination by visual confrontation, absence of deficits of understanding and alteration of verbal fluency.
- In intermediate stages there is a reduction in the number of words and verbal fluency, and an alteration of joint agility. Alteration of repetition, slight decrease in syntactic complexity, reduction of the melodic line and length of the sentence, alteration of the grammatical form without objecting to agramism, increase in the number of semantic paraphasias with slight difficulty to find words in spontaneous language and a moderate alteration of understanding. Writing is also affected.
- The evolved disease affects later areas of the caudatory and portions of the whorem that receive direct projections of the higher temporal circumvolution. Linguistic alterations with characteristics of a Wernicke aphasia. Marked reduction of verbal fluidity and the syntactic complexity of prayers in their spontaneous language, presence of verbal stereotypics or perseverance without ecolalia, alteration of repetition, marked deficits in the capacity of understanding, and important increase in the production of semantic paraphasias. The writing appears disgraphic, unpredictable shakes can occur, the syntax becomes incomplete and omissions or lexic substitutions are given. Finally, there is a marked alteration of reading characterized with multiple self-corrections, substitutions, addition of letters and words, omissions and indecision in the reading production.
Disturbations in visuospatial processing are evident in HD patients and are distinguished from visuospatial disturbances that are present in other dementias. They manifest both in initial stages and in those of moderate cognitive deterioration. They show alterations in general visuospatial processing, perceptual-motor integration, manipulation of spatial information, mental spatial rotation, sense of direction, visuospatial discrimination, and egocentric spatial perception, with preserved judgment. visuospatial. Some individuals are unable to recognize faces.
Genetics
Discovery of the gene
In 1983, six research groups, including James Gusella's, managed to isolate the huntingtin gene. This disease is one of the first in which molecular genetic methods helped discover a DNA marker linked to the gene, which allows presymptomatic and even prenatal diagnosis of some individuals. Gussella et al.'s research was one of the first to succeed in using RFLPs (Restriction Fragment Length Polymorphisms) to demonstrate linkage and it was with Huntington's disease.
At the beginning of the investigation, attempts were made to identify linkage with protein markers in serum, but this did not work. Then, a considerably large population was found to suffer from the disease in most of its members in Barranquitas and Lagunetas, Venezuelan villages close to the city of Maracaibo in Venezuela. Thanks to DNA samples donated by its members and luck (at this time there were few DNA polymorphic markers available) a marker was found. The G8 probe, which was one of those used, found two polymorphisms with the Hind III restriction enzyme. The relationship between the disease and the marker locus has been demonstrated, and it has been established that G8 maps 3 to 5 cM of the huntingtin gene.
Thanks to this great discovery in the efficacy of RFLPs in disease gene mapping, every day there are more monogenetic disorders that can be located in a specific chromosomal region. The importance of this lies in the fact that it provides the opportunity, for the first time in many cases, to make presymptomatic or prenatal diagnoses in individuals at risk.
Huntingtin gene
The huntingtin gene (HTT or IT15) was physically mapped to the most distal band of human chromosome 4, determining its location in that region. This is a rather complicated area to study because it is very close to the telomere of the short arm of the chromosome. The gene is located exactly at 4p16.3. This region is approximately 1,000 kb and has a potential gene content of about 5,000 genes of which 27 are suspected to be disease-related. The huntingtin gene produces a protein called "huntingtin" whose function is focused on neurogenesis by helping in the orientation of sister chromatids and as a regulator of apoptosis.
After managing to isolate the gene, a connection was found with many other hereditary diseases: the mutation mechanism in all of them is the expansion of trinucleotide repeats. In Huntington's disease, the increased number of triplets at a particular position in the gene is what differentiates the mutated huntingtin gene from the normal gene. At the 5' of the gene is where the triplet repeat group (CAG) is located. The triplets are located in the first exon and code for the amino acid glutamine. Normal protein is polymorphic for a polyglutamine segment. Triplet repeats typically range from 8 to 35, with 35 being considered a threshold and disease thereafter. 35 is an inaccurate threshold, since there are exceptional cases in which the minimum levels of some patients overlap with the maximum levels of the disease. Before the threshold, we can see cases of intermediate numbers of repeats that may imply a predisposition to suffer from the disease (premutation) in the next generation.
The huntingtin protein
The gene encoding the protein is highly conserved and is ubiquitously expressed throughout the body, during development when it plays an essential role, and also in postmitotic neurons and other cell types with or without neuronal origin. The protein is found in both the nucleus and the cytoplasm and is associated with various organelles and structures, including the microtubule network.
In addition, this protein is present in high concentrations in dividing cells, and is associated with essential proteins for the formation and orientation of the mitotic spindle, the main ones being those that make up the dynein/dynactin complex. It has been observed that the absence of the huntingtin protein (or, in its case, the defective protein) causes the inability of these protein complexes to orient the spindle.
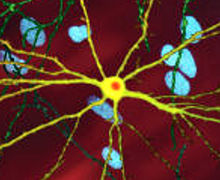
Proteins with excessively long polyQ regions are prone to misfolding and formation of inclusion bodies by amyloid aggregates. These inclusion bodies have been located both in the nucleus and in the cytoplasm of neurons, and neuronal projections from the striatum, cerebral cortex, cerebellum, and spinal cord.
Variation of the symptoms of the disease depending on the number of CAG trinucleotide repeats
It has been found that there is a highly significant negative correlation between the age of onset of the disease, defined as the age at which the first well-defined disorders appear, and the length of the CAG repeats. It has even been observed that it appears more and more prematurely with each new generation, which inherits the disease from one of the parents. This is explained because DNA polymerase, when replicating the CAG region, adds a few more repeats by default; Therefore, each generation presents a higher number of repetitions and they begin to experience the symptoms of the disease at an earlier age. There is also a negative, although less significant, correlation between the length of these repeats and the age of death.
Pathology
From the anatomopathological point of view, it is known that what happens is a neuronal degeneration and that more specifically it begins in the medium neurons (in the medium spiny neurons), conserving the large neurons. Severe and visible damage occurs in the striatum (in the lenticular nucleus and the caudate nucleus) of the brain, that is, atrophy of the brain in the parietal and frontal areas, and in the thalamus and putamen mainly. The cerebral cortex remains more or less well until the disease is quite advanced and as far as the cerebellar cortex is concerned, it has not been seen to suffer any morphological damage. Involuntary movements reveal the location of damage in the extrapyramidal system. In summary, it can be said that cerebral atrophy is produced, characterized by neuronal death and gliosis.
Gene mutation and its mechanism
The huntingtin gene is expressed in various tissues, with normal huntingtin predominating in the brain. The location of the protein in the organism has been established by means of immunohistochemistry (with monoclonal antibodies) and it has been detected in the neuronal cytoplasm, the perikaryon, the nerve fibers and the synaptic endings. For this reason, although the function of the normal protein is unknown, it is shown that it must be a structural protein of nerve endings and not a transcriptional regulator. It has been seen that Huntington's patients produce both the mutated and the normal protein and the conclusion reached is that dominance translates into a gain of function by the protein and therefore there are hardly any clinical variations between homozygous and heterozygous. The role of the mutated protein is related to brain atrophy and degeneration of medium spiny neurons, first in the putamen and then in the brain as a whole. Recent studies in this regard show that the polyglutamine amino-terminal end of the mutated protein is recognized as abnormally folded and is attacked by specific caspases to remove that end. This would cause the remains to group together and accumulate. These accumulations would cause problems and hinder regulation in the nucleus of the cell, worsening with age. In summary, the accumulation would be toxic for the cell, interrupting the protein degradation activity of the cells, which already decreases with age, and would have a cumulative effect.
It is known that the huntingtin gene mutation has not produced other variations, that is to say that other mutations in the huntingtin gene are rare, so it is believed that the emergence of the known mutation and therefore of the disease, was due to a progressive advance in the elongation of the repetition zone until the threshold was exceeded. The mutation has been maintained by transmission from generation to generation, in most cases.
Treatment
There is no treatment that cures the disease or prevents its progression. The available medication is limited to counteracting the symptoms, as well as brain surgery can considerably slow down the progress of the disease.
Against motor disorders, neuroleptics such as tiapride and tetrabenazine are prescribed which, although initially aimed at schizophrenic psychosis, secondarily limit the movements of the patients. Dopamine blockers (phenothiazine, haloperidol) and other drugs (amantidine, reserpine) are also used.
For mental disorders, antidepressants, sedatives, and antipsychotic neuroleptics are used.
In addition, there is a rehabilitation, psychiatric and psychological, nutritional and, above all, social support treatment.
If pharmacological treatment is initiated, starting doses of neuroleptics should be low, for example, 0.5-1 mg/day of haloperidol or fluphenazine. Doses can be gradually increased in small increments (1 mg/day) until symptoms are relieved. With serum concentrations of 2-5 ng/ml improvement appears, and correspond to a daily dose of 1.5-10 mg/day. Doses >10 mg/day of haloperidol produce only little or no benefit than lower doses. If patients present with rigidity, akathisia, or dystonic reactions to haloperidol or fluphenazine, less potent drugs such as thioridazine may be better tolerated. However, less potent neuroleptics are more sedating, more anticholinergic, and may cause more postural hypotension than more potent ones.
A wide variety of drugs have been used to control rigidity, spasticity, and dystonia, but without much success. An exception is botulinum toxin (IM), which has been used quite successfully for cervical dystonia in juvenile HD.
Clonazepam and valproate have been used for myoclonus; and valproate may be particularly effective in young HD patients with epilepsy rather than in those with primary generalized seizures. As with other compulsive seizures, those secondary to HD should be evaluated with an EEG.
Treatment of psychiatric disorders
Most HD depressions respond to treatment of idiopathic depression. In general, HD depression is underdiagnosed and undertreated. Although there are no controlled studies, both tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) may be effective. MAOIs have also been used with success. SSRIs are more convenient to handle because they do not require monitoring of blood levels, have a very low potential for mortality in cases of overdose, and often have the additional benefit of improving symptoms of irritability and aggression. With these drugs, patients can develop akathisia and a worsening of their insomnia, even in rare cases increasing dyskinesias. Among the tricyclic antidepressants, nortriptyline is preferred. Its low anticholinergic activity leads to less dry mouth, less constipation and less blurred vision. Its low alpha-blocking activity minimizes orthostatic hypotension.
Patients with HD may not need pharmacological treatment in seasons of good evolution if they are brief and there are no associated dangerous behaviors. Carbamazepine or sodium valproate are the initial treatment of choice, starting with small doses, gradually increasing it until a response appears.
In the treatment of irritability, the SSRIs and carbamazepine have been successful.
Sexual disturbances in HD, particularly hypersexual aggression, can be treated with antiandrogens.
Obsessive-compulsive disorders in HD can be treated with standard drugs in the treatment of obsessions, such as SSRIs and clomipramine.
Therapeutic research
Pharmacological research
Researchers' search is focused on discovering substances that slow down, if not prevent, the process of neuronal degeneration. An example of these would be glutamine receptor antagonists, which hinder the release of the glutamate transmitter.
An antibiotic, minocycline (used against acne), is effective when it comes to inhibiting caspases, which are the enzymes that trigger necrosis of nerve cells (it has already been shown to be effective in mice).
In order to prevent the degradation of the huntingtin protein, research is being done on substances such as trehalose (a sugar from desert plants) that would delay the onset of the disease.
It has also been used to intervene in the cell's altered energy metabolism, using substances from the patient's body (coenzyme Q, antioxidant, and creatine, energy store). Animal trials are encouraging.
The use of antitumor drugs is another line of therapeutic research; phenylbutyrate could work by putting protein synthesis back into operation, which is disrupted by modified huntingtin.
Gene Therapy Trials
Since this disease is due to the mutation of a single gene, the development of gene therapies is somewhat more viable than if it were a multigenic disease.
The main achievement in this area has been to prevent the expression of the modified huntingtin gene in mice, by injecting small fragments of RNA into the brain that matched the information-carrying RNA to make the pathologically altered protein and block it.
A company is currently developing a treatment for Huntington's disease. This is still in the experimental phase. It is based on the use of a technique known as zinc finger proteins (Zinc Finger Proteins, ZFP) with a strategy that tries to decrease the levels of htt repeats, while preserving the levels of the normal protein.
History and endemics
- In the past, it was not diagnosed as such (then the problem that many individuals are not aware of their family history).
- In the Medievo, this and other similar diseases (Korean of Sydenham) were known as "The Dance of St.Vitus", because the people complained of the characteristic spasmodic movements that hinder the march were pilgrims to the chapel of St.Vitus, built in Ulm (Germany), waiting for the saint to intercede for them.
- There are entire communities on the American continent where the disease is an endemic evil (because it was brought by the first colonizers); in the region of the western coast of the Lake of Maracaibo in Venezuela the number of cases exceeds up to ten times the world average.
People with Huntington's
- Woody Guthrie, American folk musician
- Thirteen, fictitious character of the series House (interpreted by Olivia Wilde)
- Poch, Spanish singer.
- Lee Gun, fictional character of the series Fated to Love You (interpreted by Jang Hyuk).
- Lee Jae-joon, fictional character of the Doctor Prisoner series (interpreted by Choi Won-young).
- Javier Maroto, fictitious character of La Que se Avecina pretends to suffer the invented disease of " Huntington-Recklinhausen syndrome"
Contenido relacionado
Aloe vera
Deinonychus antirrhopus
Calcium carbonate