Human heart
The heart (from Latin cor) is the main organ of the human circulatory system. It is a hollow, muscular, thick-walled, contractile organ that functions as a suction and delivery pump propelling blood through the arteries to distribute it throughout the body. It is located in the center of the thoracic cavity flanked on either side by the lungs.
It is the size of a fist, weighs between 250 and 300 grams in women and between 300 and 350 grams in men, which is equivalent to 0.40% of body weight. The medical specialty that studies its conditions is called of cardiology.
Anatomy
Location
The heart is a hollow muscular organ whose function is to pump blood through the body's blood vessels. It is located in the central region of the thorax, in the middle and lower mediastinum, between the two lungs. It is surrounded by a thick fibrous membrane called the pericardium. The heart is in the shape of a tilted pyramid, the pointed portion of the pyramid tilting to the left and downward, while the base faces upwards and is the area where the large blood vessels that carry blood out of the organ arise. The lower part of the heart rests on the diaphragm while the lateral aspects are contiguous with the right and left lung and the anterior aspect lies behind the sternum.
Chambers or chambers of the heart
The heart is divided into four chambers or cavities: two upper ones, called the right atrium (right atrium) and the left atrium (left atrium); and two lower ones, called the right ventricle and the left ventricle. The atria receive blood from the venous system and transfer it to the ventricles, from where it is pumped into the arterial circulation.
- Right heart. The right atrium and the right ventricle form the right heart. The right atrium receives the blood that comes from the whole body through the upper vena cava and lower vena cava. The right ventricle drives non-oxygenated blood to the lungs through the pulmonary artery.
- Left heart. The left atrium and the left ventricle form the left heart. It receives oxygenated blood from the lungs that flows through the four lung veins in the left atrium. The left ventricle drives oxygenated blood through the aorta artery to distribute it throughout the body.
The tissue that separates the right heart from the left is called the septum. Functionally it is divided into two non-separated parts: the superior, or interatrial septum, and the inferior, or interventricular septum. The latter is especially important, since the bundle of His runs through it, which allows the electrical impulse to be carried to the lowest parts of the heart.
Large glasses
The largest and most important blood vessels in the body enter or leave the heart. They are the following:
- Arteries
- Arteria aorta. It emerges from the left ventricle, it has about 3 cm in diameter at its beginning and gives origin to all blood branches that bring blood to the internal organs, muscles, and the rest of systems.
- Pulmonary artery. It emerges from the right ventricle, has 2.5 cm in diameter and carries the blood to the lungs for oxygen.
- Venas
- Vena cava superior. It flows into the right atrium, carries the venous blood from the head, neck, chest and upper limbs.
- Vena cava inferior. It flows into the right atrium, carries the venous blood from the abdomen, pelvis and lower limbs.
- Pulmonary veins. The four pulmonary veins each have a diameter of about 15 mm, flowing into the left atrium and carrying oxygenated blood from the lungs.
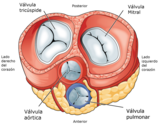
Heart valves
The heart valves are located in the outlet ducts of the four chambers of the heart, where they have the function of preventing blood from flowing in the opposite direction. They are located between the atria and ventricles or between the ventricles and the arteries of exit. They are the following four:
- tricuspid valvewhich separates the right atrium from the right ventricle.
- lung valvewhich separates the right ventricle from the pulmonary artery.
- mitral or bicuspid valvewhich separates the left atrium from the left ventricle.
- aortic valvethat separates the left ventricle from the aorta artery.
The tricuspid and mitral valves have fine extensions called chordae tendineae, they act as tensioners and serve to prevent the valve components from prolapsing towards the atrium when the ventricle contracts. The chordae tendineae attach to projections on the wall of the ventricle called the papillary muscles. The tricuspid valve consists of 3 leaflets and the mitral valve has two, which is why it is also known as the bicuspid valve.
The pulmonary and aortic valves have three leaflets each with a crescent shape, which is why together they are called semilunar or sigmoid valves, they do not have chordae tendineae.
Layers of the Heart
From the inside out, the heart has the following layers:
- Endocardio. It covers the inner cavities of the heart, both atria and ventricles. It is formed by an endothelial layer, in contact with the blood, which is continued with the endothelium of the vessels, and a layer of lax connective tissue which by its location is called subendocárdic.
- Myocardio. It is the widest layer and represents most of the thickness of the heart. It is formed by muscle tissue in charge of boosting blood by contraction. The myocardial width is not homogeneous, it is much higher in the left and lower ventricle in the right ventricle and atriums. Most of the cells that make up the myocardial are cardiomyocytes, contactal muscle cells with a cylinder that contain myophobic cells of the same characteristics as those of the striated muscle. There are also myoendocrine cells in the myocardium that in response to excessive stretching secrete the atrial natriuretic peptide that acts decreasing blood pressure. On the other hand, the driving system of the electrical impulses of the heart consists of modified cardiomyocytes specialized in this function.
- Pericardio. It is a fibroserous membrane that envelops the heart by separating it from neighboring structures. It forms a kind of bag or bag that completely covers the heart and extends to the roots of the large vessels. It is divided into a visceral layer in contact with the myocardial and a parietal layer, between both is the pericardial cavity that contains a small amount of fluid that facilitates the sliding of the two layers (pericardial fluid).
Vascular supply of the heart
The heart requires oxygen and nutrients so that the myocardium can carry out its work of contraction, the blood supply to the heart cells is carried out through the two coronary arteries, the right and left coronary arteries, both are the first branches that emits the aorta artery.
The right coronary artery begins its course in the anterior face of the heart, between the atrium and the right ventricle, then passes to the posterior part of the heart and becomes the posterior descending coronary artery that supplies blood to the posterior part of the heart. left ventricle.
The left coronary artery, after arising from the aorta, immediately divides into 2 branches called the left anterior descending coronary artery and the circumflex artery.
- The anterior descending coronary artery runs through the anterior surface of the heart and brings blood to the previous wall of the left ventricle.
- The circumflex artery runs through the space between the atrium and the left ventricle and gives rise to several branches that nourish the anterior and lateral wall of the left ventricle.
Innervation of the heart
The heart receives nerve fibers from the sympathetic nervous system and the parasympathetic nervous system.
The fibers of the sympathetic nervous system come from the cervical sympathetic ganglia from which the superior, middle, and inferior cervical cardiac nerves originate. Upon reaching the heart these nerves branch and form the sympathetic cardiac plexuses.
The fibers of the parasympathetic nervous system reach the heart from the vagus nerve. When they reach the organ, they branch off, forming a nerve plexus.
Embryology
The circulatory system is the first functional system of a vertebrate embryo. The fetal heart manifests activity from the third week of embryonic development. Heart formation begins in the primitive streak of the embryo from cardiogenic cells of the mesoderm. The transformation of the mesoderm into cardiogenic tissue depends on several proteins produced by the endoderm, including bone morphogenic protein (BMP) and fibroblast growth factor 8 (FGF-8). By the 5th week the heart rate of the embryo it is between 60-80 beats/min, it rises progressively until it reaches 180-200 beats/min in the 10th week.
The primitive cardiac tube gives rise to a structure known as the cardiac loop, which is made up of 4 parts in the caudo-cranial direction: sinus venosus, primitive atrium, primitive ventricle and bulbus arteriosus, the latter giving rise to the trunks of the great arterial vessels. To give the heart the correct shape, the cardiac loop performs a folding that causes the primitive atrium to be above the primitive ventricle.
Between day 27 and 37 of intrauterine life, four processes of internal septation of the heart occur, definitively forming both ventricles and atria, and dividing the pulmonary artery from the aorta, these processes are as follows:
- Atrioventricular stool. Separate the atriums of the ventricles.
- Interauricular stool. Separate the right atrium on the left.
- Interventricular stool. A septum or septum separates both ventricles.
- Stoconal stool. It gives origin to the aorta artery and pulmonary artery, forms a partition separating both arteries and finding them in their respective ventricle.
Physiology
The heart as a bomb
The circulatory system is made up of blood vessels that carry blood away from the heart and back to the heart. Arteries carry blood from the heart to the rest of the body, and veins carry blood from the body to the heart.
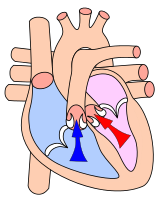
The heart is a self-controlled muscular organ, a power pump made up of two pumps in parallel that work in unison to propel blood to all organs of the body. The atria are receiving chambers, which send the blood they receive to the ventricles, which function as ejection chambers. The complete circuit consists of the following steps:
- The right atrium receives little oxygenated blood from the different organs through the lower vena cava and the upper vena cava.
- The right atrium transfers the blood to the right ventricle through the tricuspid valve.
- The right ventricle drives blood through the lung valve into the lung artery and lungs.
- The blood is oxygenated by the lungs and returns to the left heart through the lung veins, entering the left atrium.
- From the left atrium the blood crosses the mitral valve and passes to the left ventricle.
- From the left ventricle, the blood is propelled through the aortic valve to the aorta artery from which many branches are broken to provide oxygen to all tissues in the body.
- Once the different organs have captured the oxygen of the blood, the poor blood in oxygen enters the venous system and returns to the right atrium through the lower vena cava and upper vena cava, closing the circuit.
Cardiac output
Cardiac output is the amount of blood pumped by each of the ventricles of the heart in one minute. Cardiac output depends on the heart rate and the volume ejected during the contraction of a ventricle (stroke volume). Thus, the cardiac output of a person with a heart rate of 70 beats per minute and a stroke volume of 68 mL would be as follows: CO = 70 x 68 = 4760 mL/minute. Throughout a person's life, the heart performs a formidable task, pumping about 7,000 liters of blood a day for many years.
Other functions of the heart
In addition to its main activity as a blood pump, the heart has other functions:
- Secretion of atrial natriuretic peptide. It is a peptide hormone released mainly by the right atrium in response to the increased distensibility of the heart chambers, acts by increasing the elimination of urine and sodium by the kidney and dilating the blood vessels (vasodilatation).
- The atrium walls have pressure sensors called sweepers.
Cardiac cycle
A cardiac cycle consists of a phase of relaxation and ventricular filling (diastole) followed by a phase of contraction and ventricular emptying (systole). Contraction of the ventricle to expel blood to the tissues is called systole. The relaxation of the ventricle to receive blood from the atria is called diastole. Ventricular systole is preceded by contraction of the atria that facilitate rapid filling of the ventricle, contraction of the atria is sometimes called presystole or atrial systole.
The cardiac cycle occurs simultaneously in the two ventricles, the fundamental difference between the right and left heart is that the right heart drives blood towards the pulmonary artery, which has a much lower pressure than the aortic artery. Therefore, the work that the right ventricle must do to pump blood is less and the myocardium of the right ventricle is less thick than that of the left ventricle.
Conduction system of the electrical impulse of the heart
Heart muscle is myogenic, which means that it electrically excites itself, unlike skeletal muscle, which requires a stimulus from the brain to contract. Rhythmic contractions occur spontaneously and at regular intervals. The electrical conduction system of the heart is made up of a group of muscle cells specialized in generating and propagating the nerve impulse. The structures that make up the system are the following:
- Synauricular nodule, also called sinus nodule. It is the one that initiates the heart impulse so it is considered the natural pacemaker of the heart. From the synauricular nodule the electrical impulse crosses the atriums and reaches the atrioventricular nodule.
- Atrioventricular node, also called Aschoff-Tawara node, is located at the height of the right atrium. From this nodule the impulse reaches the ventricles through the atrioventricular fascicle.
- Auriculoventricular phase is the only way the nervous impulse passes from the atrium to the ventricle. It consists of His fascicle that is divided into the right and left branches and branched into the Purkinje fibers.
The distribution of the conduction system causes simultaneous contraction of the two ventricles from the region of the apex to the base.
The electrical activity of the heart can be analyzed with electrodes located on the surface of the skin, this technique is used for medical diagnosis and is called electrocardiogram, ECG or EKG.
Heart rate
The heart rate at rest usually ranges between 60 and 80 beats per minute, however frequencies outside this range are considered normal in many cases, trained athletes can have rates of 50 beats per minute or even lower, on the contrary people normal in a state of anxiety or nervousness may present frequencies higher than 110 beats per minute.
Although the heart generates its own impulses in the sinoatrial node, heart rate is also determined by other factors, including adrenaline produced by the adrenal glands and nerve impulses from the sympathetic and parasympathetic nervous systems. Sympathetic nerve fibers produce stimuli in response to an alarm reaction or increased physical activity, these stimuli act on the sinoatrial node and cause increased speed of myocardial contraction with increased heart rate, also directly influence muscle fibers of the myocardium increasing the force of contraction. On the contrary, the stimuli of the parasympathetic nervous system have an opposite action, they act on the heart through the vagus nerve and decrease the heart rate by slowing down the impulses generated by the sinoatrial node. In this way, the heart can easily adapt to changing needs and increase or decrease the volume of blood it propels as needed by the body.
Properties of the heart
The heart muscle has four fundamental properties:
- Batmotropism: Also called excitability, is the ability of the muscle cells of the heart to depolarize and generate a potential for action against the arrival of an electrical stimulus.
- Inotropism: Also called contractibility, refers to the contractable capacity of the heart. It is said that a drug has a positive inotropic effect when it improves the capacity of contraction, on the contrary the negative inotropic effect indicates a decrease in this capacity.
- Chronotropism: Also called automatism, refers to the ability of the heart to automatically generate action potentials to a certain frequency that causes periodic contractions. It is said that a stimulus or substance has positive chronotropic effect when it increases the heart rate and negative chronotropic effect when it decreases.
- Dromotropism: The term dromotropism or conductibility refers to the ability of the heart to perform the transmission of electrical impulses through the electrical driving system of the heart.
Heart sounds
When a stethoscope is used to listen to the sound made by the heart, two noises can be distinguished:
- The first of these sounds corresponds to the contraction of the ventricles and the closure of the atrioventricular valves (mitral and tricuspid);
- The second sound corresponds to the relaxation of the ventricles and the closure of the lung and aortic valves.
Diseases
Cardiovascular disease is the leading cause of death worldwide. The heart diseases that globally represent a major health problem are ischemic heart disease and heart failure.
- Ischemic cardiopathy. It is due to the decrease in the blood flow that the heart receives through the coronary arteries as a result of arteriosclerosis; within ischemic heart disease is included angina of the chest and myocardial infarction. The main known risk factors are smoking, obesity, diabetes mellitus, high cholesterol and high blood pressure.
- Heart failure. It is the ultimate consequence of most heart disease and can be acute or chronic; the latter is a long-term disorder that has regular decompensations or aggravations and is an important cause of mortality and hospital admission.
- Congenital cardiopathies. Set of heart disease and large vessels that originate before birth during intrauterine life. Most are due to defective embryo development during pregnancy, when the main cardiovascular structures are formed. Some produce mild disorders, but others are very serious and incompatible with life; among the most common are interauricular communication, interventricular communication, persistent artery ductus, aorta coartation and Fallot tetralogy.
- Valvulopathies. They are all diseases that affect heart valves; they can be divided into stenosis, when the light of the valve is narrowed which makes it difficult to pass the blood, or insufficiency, when blood regurgitation occurs in the reverse sense. Examples of valvulopathies are aortic stenosis and mitral insufficiency.
- Arrhythmias. Heart arrhythmias, or rhythm disorders, are any alteration that occurs in the normal sequence of contraction and relaxation of the heart. There are many types of arrhythmia, and their severity and clinical consequences are very diverse. In some cases they go unnoticed, however certain types have important effects on heart function. Examples of arrhythmia are atrial fibrillation, ventricular extrasystole and ventricular fibrillation.
Diagnostic procedures
- Auscultation. Abscation can detect abnormal sounds of the heart and the existence of breaths. The blows are sound waves of a frequency between 20 and 2000 hertziums that occur as a result of turbulence in the blood flow of the heart or blood vessels. They may be due to a valve lesion, an abnormal communication between the right and the left heart or other causes. Determined breaths are not the result of disease and are called functional blows
- Electrocardiogram. It consists in the paper record of the electrical activity of the heart. It is done by placing several electrodes on the skin and detecting potential differences between them. The record obtained in this way is widely used in diagnostic medicine and provides numerous data especially useful for the detection of heart rhythm disorders, known generically as arrhythmias.
- Echocardiography. This technique uses ultrasounds to obtain high-precision heart images that enable both heart anatomy and its alterations as well as organ function. Failure to use ionizing radiation does not cause adverse effects. It is an inocuous, painless and highly useful procedure in cardiology.
- Electrocardiography Holter. It consists of the outpatient monitoring of the electrocardiographic registry for a long time, usually twenty-four hours, in a person on the move.
- Heart MRI. It is the application of magnetic resonance to the field of cardiology. High-quality images are obtained without invasive procedures. It allows to study both the function and the anatomy of the heart and has some advantages over echocardiography. It has a good ability to differentiate tissues without using intravenous contrast.
- Ergometrics. Also called stress test, it is to perform a continuous electrocardiogram record during the realization of a controlled effort, in order to detect alterations that are not visible in resting state. It is mainly used for the diagnosis of ischemic heart disease.
- Heart rate. It is a procedure for diagnosis or treatment that consists of inserting a catheter into the vascular system, which makes progress to cardiac cavities and coronary arteries.
- Coronary. It consists in the intravascular administration of a radiopaque contrast in the coronary arteries; after the injection of the contrast, the coronary arteries can be seen, by x-rays, and visualize stenosis or obstructions in it. The technique requires a cardiac catheterization as a previous step.
Contenido relacionado
Chrysopogon
Colacium
Apoclate simplex