Cardiac cycle
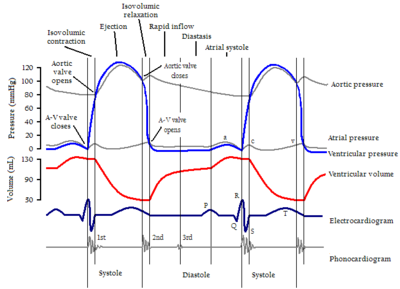
The cardiac cycle is the sequence of mechanical, sound and pressure events related to the flow of blood through the cardiac chambers, the contraction and relaxation of each of them (atria and ventricles), the closing and opening of the valves and the production of noises. This process takes less than a second. The reciprocal of the duration of a cycle is the heart rate (as it is usually expressed in beats per minute, multiply by 60 if the duration is measured in minutes).
Phases of the cardiac cycle
In each beat there are five phases:
- Active ventricular filling (systole atrial).
- Isovolumetric ventricular contraction.
- Eyection.
- Isovolumetric ventricular relax.
- Passive headphone.
The first three correspond to systole.
- Active ventricular filling (atrial sistole)
The cycle begins with an action potential in the sinus node that will initially propagate through the atria causing their contraction. When these contract, all the blood they contain is expelled into the ventricles. This is possible thanks to the fact that in this phase, the atrioventricular (mitral and tricuspid) valves are open, while the sigmoid (aortic and pulmonary) valves are closed. At the end of this phase; all the blood contained in the heart will be found in the ventricles, giving way to the next phase.
Isovolumetric ventricular contraction
The wave of depolarization reaches the ventricles, which consequently begin to contract. This causes the pressure to increase inside them, in such a way that the ventricular pressure will exceed the atrial pressure and the flow will tend to go back towards the latter. However, this does not happen, since the increase in ventricular pressure determines the closure of the atrioventricular valves, which will prevent the retrograde flow of blood. Therefore, in this phase all the heart valves will be closed.
Ejection
The ventricular pressure will also be greater than the arterial pressure in the great vessels leaving the heart (pulmonary trunk and aorta) so the sigmoid valves will open and flow will pass from the ventricles into the lumen of these vessels. As the blood leaves the ventricles towards them, the ventricular pressure will decrease at the same time that it increases in the great vessels. This ends up equalizing both pressures, so that part of the flow does not pass, due to a pressure gradient, towards the aorta and pulmonary trunk.
The volume of blood that remains retained in the heart at the end of the ejection is called the residual, end-systolic or end-systolic volume; while the volume of blood ejected will be the stroke volume or stroke volume (approximately 70 mL).
Isovolumetric ventricular relaxation
Corresponds to the beginning of diastole or, what is the same, to the period of myocardial relaxation. In this phase, the ventricle relaxes, in such a way that this fact, together with the partial output of its flow (occurring in the previous phase), causes the pressure inside it to drop enormously, becoming less than the normal pressure. of the great vessels. For this reason, the blood flow becomes retrograde and begins to occupy the aortic and pulmonary sinuses of the sigmoid leaflets, pushing them and causing them to close (as blood fills the aortic sinuses, part of the flow will pass to the coronary arteries, originating from them). This stage is therefore defined as the interval that elapses from the closure of the sigmoid valves to the opening of the atrioventricular valves.
Passive atrial filling
During the processes discussed above, the atria will have been filling with blood, so that the pressure in them will also be higher than in the ventricles, partially emptied and relaxed. The pressure gradient itself will cause blood to flow from the atria to the ventricles, pushing the mitral and tricuspid valves, which will open allowing flow in this direction. A new atrial contraction originating from the sinus node will end this phase and initiate atrial systole of the next cycle.
Factors
It is important to remember that there are several determinants of cardiac function that can alter the phases of the cycle: preload, afterload, inotropy, compliance, and rate.
- The preload depends on the volume of the ventricle at the end of the diastole (VFD).
- Postload represents the aortic pressure against which the ventricle must contract.
- Inotropism corresponds to the intrinsic force that generates the ventricle in each contraction as a mechanical pump.
- Distensibility refers to the ability of the ventricle to expand and fill in during the diastole. (Frank-Starling Law)
- Heart rate is the number of heart cycles per time unit.
The cycle repeats itself about seventy-two times per minute, but can be increased or slowed down according to the body's needs through the nervous system.
Heart sounds
For each beat, the heart makes two heart sounds (lub-dub) separated from each other by a silence.
Closing of the mitral and tricuspid valves (called atrioventricular valves) at beginning of systole causes the first part (lub) of the auscultatory sound (lub- dub) heard when the heart contracts. Formally, that first sound is known as the first heart sound, or S1. That first heart sound is created when the mitral and tricuspid valves close and actually has two components, one mitral (M1) and one tricuspid (T1).
The second portion of the lub-dub—the second heart sound, or S2—is caused by the closure of the aortic and pulmonic valves at the end of ventricular systole. As the left ventricle empties, its pressure falls below the pressure in the aorta, so the aortic valve closes. Similarly, when the pressure in the right ventricle falls below the pressure in the pulmonary artery, the pulmonary valve closes. The second heart sound also has two components, an aortic (A2) and a pulmonary (P2) component. The aortic valve closes before the pulmonary valve and therefore they are audible separately from each other on the second heart sound.
Electric drive system
The heart's pumping action comes from an intrinsic electrical conduction system. The electrical impulse is generated in the sinus node or sinoatrial node, which is a small mass of specialized tissue located in the right atrium of the heart. The electrical impulse will then travel to the atrioventricular node, where the impulses are delayed for a brief instant, and then continue along the conduction pathway through the bundle of His (which divides into a right and a left branch) toward the ventricles. The conduction pathway ends in a series of fibers called Purkinje fibers.
The ability of the heart to generate an electrical impulse resides in the cells that form it. These cardiomyocytes are self-excitable, which means that they do not require the presence of an external stimulus to generate a contractile response; and rhythmic which allows them to maintain a sufficient contraction frequency to maintain the pumping activity without stopping.
The sinus node (also called the sinoatrial node) is made up of a group of atrial fibers with the highest rhythmicity. For this reason, their activity is what sets the basic frequency of the heart and they are called pacemaker cells. This nodule regularly generates an electrical impulse 60 to 100 times per minute under normal conditions. The action potential will propagate through cardiac cells thanks to existing gap junctions between them. In this way, the depolarization initiated in the sinus node spreads through all the atrial fibers from top to bottom, through four bundles that leave the node:
- The first three run through the right atrium, and are the previous branch, middle branch and rear branch
- The fourth branch is the branch for the left atrium, and goes to this place.
In this way the right and left atria are stimulated first and contract for a short period of time before the rest of the cavities do. Depolarization reaches the atrioventricular node, located in the cardiac cross (located at the junction of the interatrial and interventricular septa with the atrioventricular septum). At this point there are fibrous rings or cardiac skeleton. There is a slowing down of the propagation (0.1 s delay) due to the geometry of the fibers. This node is characterized by being a narrow beam with few gap-type junctions, therefore the conduction velocity of the impulse is lower and this delay is given.
The potential then moves rapidly through the bundle of His, which will divide into a right limb and a left limb >. These branches run through the entire interventricular septum. Its function is to generate the contraction of the septum. Finally, the Purkinje fibers or subendocardial network travel through the free walls of the right and left ventricle to generate ventricular contraction.
Pressure curves
Atrial pressure curve
The atria undergo a series of changes in their pressure according to the different phases of the cardiac cycle:
Wave “a”: corresponds to the contraction of the atria (atrial systole).
“C” wave: it is caused by the bulging of the valve plane towards the atrium when the ventricle contracts (isovolumetric ventricular contraction).
Sinus “x”: this is a drop in pressure in the atria due to displacement of the valve plane toward the apex during ventricular ejection (ejection).
“V” wave: blood reaches the atrium, which implies an increase in pressure (isovolumetric ventricular relaxation).
Sinus “y”: the atrioventricular valve opens, which implies a drop in atrial pressure due to the emptying of blood into the ventricle (passive ventricular filling).
Ventricular pressure curve
- During the symstole headphone, ventricular pressure increases by the arrival of blood due to the contraction of the atrium.
- This pressure continues to increase during isovolumetric ventricular contract until the moment it exceeds that of the sigmoid valves.
- With the opening of the sigmoid valves takes place ejection from blood to big glasses. The pressure continues to increase by the contraction of the ventricle and begins to descend once it has emptied, so that the sigmoid valves are also closed when the pressure in the ventricle is lower than in the large vessels.
- With the beginning of the diastole (ventricular relaxation isovolumetric) the pressure continues to decline until it becomes less than in the atrium, at which point the aurcle-ventricular valves are opened.
- With the opening of the valves, the passive ventricular filling and, therefore, the progressive increase in pressure.
Pressure curves in the aorta and pulmonary artery
The sigmoid valves open when the pressure in the ventricles is higher than that of the great vessels, that is, they open during ejection and empty the blood, so that from their opening to closing, the ventricle and the corresponding artery share pressure, so the pressure graph is identical for both. Once the valve closes, the pressure gradually drops, since the arterial wall is elastic.
If a graph is drawn comparing the pressure against the volume of the left ventricle, the result that we will obtain is a cyclical curve. Both in systole and diastole, left ventricular pressure depends on the volume it contains inside and on compliance. That is, a ventricle has increased pressure if it is poorly compliant or if it has an increased volume of blood inside it. Cyclic phenomena can be studied from any point of it. The main electrical, mechanical and sound events, correlated in the pressure volume curve can be summarized as:
- Ventricular diastole
- At the end of a contraction the ventricle relaxes (at this point is the isometric relaxation in which there is a change of pressure without volume change).
- When the pressure of the ventricle is lower than in the left atrium, the mitral valve is opened and the ventricle begins to be filled in two phases: fast filling and slow filling. In some pathological conditions there is a third noise during the rapid filling phase.
- Before the filling is finished, the P-wave occurs in the ECG, then the atrium is contracted and the A-wave occurs in the venous pulse curve. In that contraction the fourth noise can be heard in certain situations. Then the mitral valve is closed, which causes the first heart noise. Just before this sound phenomenon occurs, the ventricle is depolarized and the ECG QRS is generated.
- Sistole ventricular
- The ventricle starts to contract and the pressure increases until the pressure in the aorta exceeds (up to this time it is called isometric contraction, because there is a change of pressure without volume change).
- At this point the aortic valve opens and begins the rapid ejection and slow blood ejection, which continues against the aortic pressure until the pressure of the ventricle decreases and becomes less than the aortic pressure. At the end of this phase, the repolarization of the ECG ventricle and wave T occurs.
- At this time the aortic valve is closed and the second heart noise is generated and the ejection ends.
EKG
On the electrocardiogram, the electrical systole of the ventricles begins where the QRS complex begins. The electrical systole of the atria begins with the onset of the P wave of the electrocardiogram (ECG).
Corresponding to the physiology of the cardiac cycle, the P wave represents the filling phase, the QRS Complex the isovolumetric contraction phase, and what corresponds to the ejection and isovolumetric relaxation phase is represented from the point where the QRS complex ends until the end of the T wave.
Referring to electrical physiology, the P wave is the representation of the onset of sinus node excitation, sinus-atrial conduction, onset of atrial depolarization, arrival of the wave at the AV node, and complete atrial depolarization. The PR segment is the representation of the arrival of the wave to the Bundle of His and then to the Purkinje fibers. The QRS complex represents ventricular depolarization, and the T wave represents ventricular repolarization.
Also; atrial repolarization occurs during the QRS complex and is masked by it.
Contenido relacionado
Atoll
Zebra
Glandular acinus