Bronchiole
The bronchioles are the small airways, one millimeter or less, into which the distal bronchial tree divides. Their number has been estimated at around 60,000 bronchioles (30,000 in each lung). The bronchioles have no cartilage and are surrounded by thin smooth muscle fibers.
The bronchioles are the last air conduction structures, and the site of obstructive disorders such as bronchospasm and bronchiolitis.
Embryonic origin
The formation of the respiratory system begins in the embryo at 4 weeks of gestation, with the appearance of the lung bud. The epithelium lining the bronchi, like that of the lungs, is of endodermal origin. The muscular and connective components are derived from the splanchnic mesoderm.
As the embryo grows, the lung bud branches to form the main, secondary, and tertiary (segmental) bronchi. 17 subdivisions originate at the end of the sixth month of gestation.
Terminal bronchioles are formed between weeks 5-16 of gestation in humans. In the next phase until week 27, each terminal bronchiole divides into 2-3 respiratory bronchioles, which in turn divide into 3-6 alveolar ducts.
Anatomy of the bronchioles
In the segmentation of the bronchial tree, the ducts from generation number 12 onwards no longer have cartilage on their walls and are called bronchioles.
The bronchioles have a descending diameter of 1-0.2 mm in the direction of the alveolus.
The number of bronchioles has been estimated at 30,000 in each lung.
Its interior is lined by an epithelium, made up of at least four types of cells, which vary in their location and number.
Segmentation
The generation #16 of the segmentation of the bronchial tree corresponds to the so-called terminal bronchiole, which is the portion of the small airway that does not yet have alveoli.
The smaller bronchioles branch into the terminal bronchioles and finally, each of them divides to form the respiratory bronchioles.
Terminal bronchiole
The so-called terminal bronchiole depends on the entire "pulmonary acinus" made up of
bronchioles, alveolar ducts, and alveolar sacs.
The terminal bronchioles, 0.5 mm or less in diameter, constitute the most distal segment and mark the end of the airflow conduction division.
The entire zone distal to the terminal bronchiole would be called the respiratory or exchange zone, and its volume is about 2,500-3,000 milliliters (ml).
Respiratory bronchiole
Corresponds to the generations of bronchioles (#17, #18, #19), with some alveoli in their walls. The respiratory bronchioles are the last and narrowest of the airways.
From the respiratory bronchiole depend:
- alveolar ducts (generation #20, #21, #22) and
- alveolar bags (generation #23).
The respiratory bronchioles mark the beginning of the respiratory sector, where the exchange of gases between the blood and alveolar air takes place.
Microarchitecture
Like the rest of the airways, the bronchiole is lined on the inside by various types of cells: basal cells, ciliated cells, goblet cells, and "Club" (or Clara).
Hair cells that favor the expulsion of microorganisms and debris from the respiratory tract.
Goblet cells, which secrete mucus that helps protect the lining of the bronchi and trap microorganisms.
Clara cells of the secretory type represent 20% of all cells in the epithelium of the human small airway.
Basal cells represent 5–10% of the cells in the small airway. These are the stem or progenitor cells of the epithelium of the proximal bronchioles. They can differentiate to replenish epithelial cells, including hair cells and secretory goblet cells.
Initially the bronchioles are ciliated and gradually change from columnar epithelium in the proximal bronchioles to simple cuboidal in the terminal bronchioles, and their inner lining no longer contains goblet cells.
Surrounding the epithelium on the outside are thin bronchiolar smooth muscle fibers. In contact are the nervous branches, arteries and veins. At this level of segmentation, the bronchioles lack a supporting cartilage skeleton.
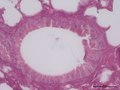
Bronchiolar histology
In bronchioles there are no subepithelial glands. This epithelium of the proximal bronchyl remains wet by a layer of mucus, segregated by caliciform cells. Caliciform cells are present in the larger bronchioles, but they are completely missing in the terminal bronchioles.
The terminal bronchioles are lined by simple cuboidal ciliated epithelium, in which Clara cells are scattered among the ciliated cells. They have 100-200 cilia per cell.
The epithelium of the distal (respiratory) bronchioles no longer contains ciliated cells and is kept moist by the lubricant secreted by Clara cells.
Bronchiolar Physiology
The main function of the bronchioles from generation number 12 of the segmentation is to lead the column of inspired air towards the alveolar portion of the bronchial tree, and in a second step allow the elimination of air outside the respiratory system.
- Decontamination of inspired air
All of the airways are kept moist by a layer of mucus that lines the surface. This mucus traps small particles from the inspired air, preventing them from reaching the alveoli, and is mobilized by the action of the cilia, which beat 10-15 times per second, towards the pharynx. The mucus, with the trapped particles, is then swallowed or coughed up.
Cell turnover in the bronchiole
Cell turnover and proliferation is relatively low in the mature bronchiole.
The epithelium of the normal adult human airway is changed approximately every 1-4 months.
Under physiological conditions the basal cells are relatively quiescent and only a few intermediate cells can be observed.
The airway Clara cell is capable of self-renewal and transdifferentiation into hair cells and goblet cells and has been termed a facultative progenitor in pulmonary homeostasis.
After severe bronchiolar injury, resident cells that play a role in repair include toxic-resistant Clara cells and bronchoalveolar stem cells, which have been proposed as relatively specialized stem cells.
An imbalance between exogenous epithelial damage and bronchiolar epithelial repair is the basis of chronic lung diseases such as asthma, COPD, pulmonary fibrosis and bronchogenic cancer.
Associated diseases
Bronchospasm
It is the narrowing of the bronchial lumen due to the contraction of the musculature of the bronchi, which causes difficulties in breathing. Almost always wheezing or wheezing, dyspnea, chest pain, or coughing occurs when inhaling air. Bronchospasms can result as a side effect of certain medications, such as beta-blockers and pilocarpine.
Bronchiolitis
It is an inflammation of the bronchioles. It is usually a symptom of a viral infection. Bronchiolitis obliterans is irreversible and may require lung transplantation in severe cases.
Asthma
It is caused by inflammation of the airways. During an asthma attack, smooth muscles located in the bronchioles contract and reduce airflow. Airflow can be further reduced by inflammation and excess mucous secretion.
Image gallery
Contenido relacionado
Poliomyelitis
Nuclear magnetic resonance
Trigynaea