Alzheimer disease
Alzheimer's disease (AD), called senile dementia of the Alzheimer's type (ADD) or simply Alzheimer's is a neurodegenerative disease, the product of a process of neurodegeneration that manifests as cognitive impairment and behavioral disorders. It is characterized in its typical form by a loss of immediate memory and other mental abilities (such as higher cognitive abilities), as nerve cells (neurons) die and different areas of the brain atrophy. The disease usually has an approximate mean duration—after diagnosis—of 10 years, although this may vary in direct proportion to the severity of the disease at the time of diagnosis.
Alzheimer's disease is the most common form of dementia, it is incurable and terminal, and it appears more frequently in people older than 65 years of age, although it can also develop in rare cases from the age of 40.
Many people experience forgetfulness or mild memory delays, which are part of the normal aging process. Most people have occasional difficulty remembering a word or someone's name. However, a person with Alzheimer's disease or other types of dementia will find these symptoms increasingly frequent and severe.
Signs of Alzheimer's disease may include:
- Changes in personality
- Deterior in movement capacity or walking
- Difficulty communicating
- Low energy level
- Loss of memory
- mood changes
- Attention and guidance problems
- Inability to resolve simple arithmetic operations
Symptoms as a defined disease entity were identified by the German psychiatrist Emil Kraepelin, while the characteristic neuropathology was first noted by the German psychiatrist and neurologist Alois Alzheimer in 1906.
So the discovery of the disease was the work of both psychiatrists, who worked in the same laboratory. However, given the great importance that Kraepelin attached to finding the neuropathological basis of psychiatric disorders, he decided to name Alzheimer's disease after his partner.
Usually, the initial symptom is the inability to acquire new memories, but it is often confused with attitudes related to old age or stress.
If Alzheimer's is suspected, the diagnosis is made with cognitive behavioral assessments, as well as neuroimaging, if available.
As the disease progresses, mental confusion, irritability and aggression, mood swings, language disturbances, short-term memory loss, and a predisposition to withdraw as the patient's senses decline.
Gradually, biological functions are lost, eventually leading to death.
The prognosis for each individual is difficult to determine. The overall average is seven years; less than 3% of patients live more than 14 years after diagnosis.
The cause of Alzheimer's disease remains unknown, although the latest research suggests that prion-type processes are involved. Research often associates the disease with the development of senile plaques and neurofibrillary tangles. Current treatments offer moderate symptomatic benefits, but there is no treatment to slow or stop the progression of the disease. However, preliminary cases of association of Alzheimer's dementia with celiac disease showed improvement with adherence to a gluten-free diet. Currently, exact diagnosis is only achieved post-mortem, so there is great interest in finding genetic markers that allow early detection of this disease, which would be easier to treat than in more advanced stages.
For the prevention of Alzheimer's, various behavioral habits have been suggested, but there is no published evidence highlighting the benefits of these recommendations, including mental stimulation and a balanced diet.
The role played by the caregiver of the subject with Alzheimer's is fundamental, even when the pressures and physical demands of this care can become a great personal burden.
International Alzheimer's Day is commemorated on September 21, a date chosen by the WHO and the International Alzheimer's Federation, in which activities are carried out in various countries to raise awareness and help prevent the disease.
The World Health Organization (WHO) held its First WHO Ministerial Conference on Global Action Against Dementia in 2015.
History
Greek and Roman doctors associated old age with dementia. But it was not until 1901 that the German psychiatrist Alois Alzheimer identified the first case of what is known today as Alzheimer's disease in a 51-year-old woman; this woman was called Auguste Deter. The researcher followed her patient until her death in 1906, and was then able to look at her brain. After this moment, he was able to publicly report the case for the first time.
One of the first symptoms of a 51-year-old woman was a strong feeling of jealousy towards her husband. He soon showed progressive memory flaws, could not find the way home, carried meaningless objects, hid or sometimes thought that other people wanted to kill it, so he started screaming.During his internment, his gestures showed complete impotence. She was disoriented in time and space. From when he said he didn't understand anything, he felt confused and totally lost. He sometimes considered the arrival of the doctor as the visit of an official and asked for forgiveness for not finishing his work, while at other times he began to scream for fear that the doctor would want to operate. Sometimes he was utterly outraged, squealing phrases that indicated his fear that the doctor would want to hurt his honor. From time to time I was completely delusional, dragging the blankets from one side to another, calling her husband and daughter, and looking like hearing hallucinations. I often screamed for hours and a horrible voice.
Mental regression gradually advanced. After four and a half years of disease, the patient died. In the end he was completely apathetic and confined to the bed, where he adopted a fetal position.Extracts from the text of Alois Alzheimer, 1907
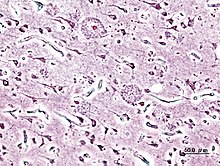
After the woman died, Alzheimer's examined her brain under a microscope. He noted changes in the "neurofibrils," elements of the cytoskeleton stained with a silver solution.
Bielschowsky's silver preparation showed very characteristic changes of neurofibrillas. However, inside the normal-looking cell one or more unique fibers could be observed that were prominent by their thickness and impregnability. At a more advanced stage, many parallel-set fibrills showed the same changes. Then they accumulated forming dense beams and gradually progressed toward the surface of the cell. Sometimes the nucleus and cytoplasm disappeared, and only a set of fibrill beams indicated where a neuron had existed. Since these fibers could be stained with stains different from normal neurofibrillas, a chemical transformation of the fibrillous substance had to have occurred. This could be the reason the fibrills survived the destruction of the cell. It seems that the transformation of the fibrillas coincides with the storage of a pathological product still not well known of the metabolism of the neuron. About a quarter or a third of all brain cortex neurons showed those alterations. Numerous neurons, especially in the high cellular layers, had disappeared completely.extracted from the text of Alois Alzheimer, 1907
During the next five years, the medical literature reported at least eleven similar cases, some of them already using the term "Alzheimer's disease". The disease was first categorized by Emil Kraepelin after deletion of some elements clinical concomitants such as delusions and hallucinations, as well as histological features irrelevant to the disease, such as arteriosclerotic changes, which were featured in the original report on Auguste D.
In the eighth edition of his psychiatry textbook, published in 1910, he included Alzheimer's disease, also called "presenile dementia" by Emil Kraepelin, as a subtype of senile dementia.
For most of the 20th century, the diagnosis of Alzheimer's was reserved for people between the ages of 45 and 65 with symptoms of dementia. The terminology has changed since 1977, when a conference on Alzheimer's concluded that the clinical and pathological manifestations of presenile and senile dementia were almost identical, although the authors also added that this did not rule out the possibility that had different causes.
This ultimately led to a diagnosis of Alzheimer's regardless of age.
The term senile dementia of the Alzheimer's type was used for a time to describe the disorder in those older than 65 years of age, while classic Alzheimer's disease was reserved for those of younger ages. Eventually, the term Alzheimer's disease was officially approved into medical nomenclature to describe individuals of all ages with a common symptom pattern: characteristic, disease course, and neuropathology.
Epidemiology
| Age | Incidence (new cases) per thousand persons |
|---|---|
| 65-69 | 3 |
| 70-74 | 6 |
| 75-79 | 9 |
| 80-84 | 23 |
| 85-89 | 40 |
| 90- | 69 |
The incidence in cohort studies shows rates between 10 and 15 new cases per thousand people per year for the appearance of any form of dementia and between 5 and 8 for the appearance of Alzheimer's.
That is, half of all new cases of dementia each year are Alzheimer's patients. There are also differences in incidence depending on sex, since there is a higher risk of suffering from the disease in women, particularly among the population over 85 years of age.
Prevalence is the percentage of a given population with a disease. Advanced age is the main risk factor for Alzheimer's: more frequent at older ages. The World Health Organization estimated that in 2005, 0.379% of people globally had dementia, and that the prevalence would increase to 0.441% in 2015 and 0.556% in 2030.
On the other hand, Alzheimer's Disease International has estimated for the year 2010 a worldwide prevalence of dementia of 4.7% for people aged 60 or over, representing upward figures by the way compared to several previously published studies (10% higher than those estimated for The Lancet in 2005). Another study estimated that in 2006, 0.4% of the world population (between 0.17-0.89%; absolute value: approximately 26,600,000, with a range between 11,400,000 and 59,400,000) was affected by Alzheimer's, and that the prevalence would triple by the year 2050.
In 2015, the First Ministerial Conference of the WHO on Global Action against Dementia estimated the number of cases worldwide at 47.5 million.
In the United States, the prevalence of Alzheimer's was 1.6% in the year 2000, both in the general population and in those between 65 and 74 years of age. There was an increase of 19% in the 75-84 age group, and 42% in the 84+ age group. However, prevalence rates in less developed regions of the world are lower.
In the European population, a meta-analysis published in 2017 in the journal Neurology revealed that the prevalence of Alzheimer's between 65 and 74 years of age is 0.97%, increasing to 7.66% in the group between 75 and 84 years, and 22.53% in the group over 85 years. This same study also confirmed that this neurodegenerative disease appears more frequently in the female sex, since women have a prevalence of Alzheimer's disease of 7.13%, while the prevalence in men is 3.31%.
Etiology
The causes of Alzheimer's have not been fully discovered. There are three main hypotheses to explain the phenomenon: acetylcholine deficiency, amyloid or tau accumulation, and metabolic disorders.
Cholinergic hypothesis
The oldest of these, and the one on which most currently available treatments are based, is the cholinergic hypothesis, which suggests that Alzheimer's is due to a reduction in the synthesis of the neurotransmitter acetylcholine. This hypothesis has not received general support for the reason that drugs that treat a cholinergic deficiency have reduced effectiveness in preventing or curing Alzheimer's, although it has been proposed that the effects of acetylcholine initiate accumulation on such large scales. leading to generalized neuroinflammation that is no longer treatable simply by promoting neurotransmitter synthesis.
Metabolic Disorders Hypothesis
Some recent research has linked dementia, including Alzheimer's disease, to metabolic disorders, particularly hyperglycemia and insulin resistance. The expression of insulin receptors has been demonstrated in the neurons of the central nervous system, preferably in those of the hippocampus. In these neurons, when insulin binds to its cellular receptor, the activation of intracellular signaling cascades is promoted, leading to a change in the expression of genes related to synaptic plasticity processes and enzymes related to the clearance of the same insulin and beta-amyloid. These insulin-degrading enzymes promote a decrease in toxicity due to amyloid in animal models.
In essence, Alzheimer's can be thought of as a form of brain diabetes that has elements of both insulin resistance and insulin deficiency. To consolidate this concept, it has been proposed that Alzheimer's be known as "type 3 diabetes".
Alzheimer's disease is associated with progressive cerebral insulin resistance in the absence of T2DM, peripheral insulin resistance, or obesity. Postmortem studies demonstrated that both molecularly and biochemically, as well as abnormal signal transduction in Alzheimer's disease, were virtually identical to what occurs in type I and type II diabetes mellitus. When locally administered pro-diabetic drugs, such as streptozotocin, they generate cognitive damage, with spatial and memory deficiency, as well as neurodegeneration typical of Alzheimer's, but they do not generate diabetes mellitus.
Aluminum Exposure
There has been controversy surrounding the role of aluminum as a risk factor for Alzheimer's disease, and this hypothesis was abandoned by many scientists in 2014.
Some studies in 2016 have shown that aluminum is associated with several neurophysiological processes that cause the characteristic degeneration of Alzheimer's. However, some people who have been chronically exposed to aluminum, through food or water, have not showing no symptoms of the disease. The probable explanation is that your intestine maintains the protective barrier function, which prevents the passage of toxic substances into the blood and the consequent reactions.
Gluten consumption
Cases of association of Alzheimer's dementia with gluten consumption and improvement with following a gluten-free diet have been documented.
Hypothesis of β-amyloid and tau proteins
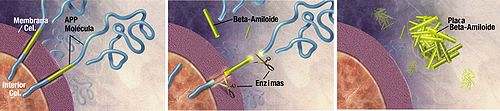
Another hypothesis proposed in 1991 has been related to the abnormal accumulation of beta-amyloid protein (also called Aβ amyloid) and tau in the brains of Alzheimer's patients.
In a minority of patients, the disease is caused by the appearance of mutations in the PSEN1, PSEN2 genes and in the APP gene, located on chromosome 21. In the latter case, the disease classically appears in people with the Down syndrome (trisomy on chromosome 21), almost universally in the 40s of life and is transmitted from parents to children (which is why there is usually a family history of Alzheimer's in patients who develop the disease at an early age). This relationship on chromosome 21, and the very high frequency of appearance of the disease in the trisomies of that chromosome, make the theory very evident.
In order to talk about presenilins, we must remember that Alzheimer's is characterized by amyloid deposits in the brain (as supported by the second theory in this article).
Its main component is the 42-amino acid beta-amyloid peptide (βA42), in whose production process the participation of γ-secretase is essential, which in turn depends on presenilins (PSEN).
In this way, a new group of molecules implicated in the genesis of Alzheimer's disease and essential for its understanding is established. In addition, they are notably topical due to the fact that their discovery is relatively recent and the possibilities they offer as therapeutic targets.
To understand what these molecules are, we must note that they are a group of peptide substances produced mainly in the brain.
There are two types, PSEN 1 and PSEN 2, with a similar structure. The main function of both PSENs is the proteolytic processing of numerous type 1 membrane proteins, including APP, as part of γ secretase; hence the importance of PSEN in Alzheimer's disease, since through the regulation of γ secretase they determine the form of Aβ that is generated and therefore its accumulation in brain tissue.
Early-onset Alzheimer's has been linked to mutations on chromosome 21, which contains the ASF gene, and chromosomes 14 and 1, which code for PSEN1 and PSEN2, respectively. These mutations result in, among other effects, increased levels of βA, whereas late-onset Alzheimer's is associated with mutations in the apolipoprotein E gene.
The gene that encodes PSEN1, of which 177 different mutations are known, is responsible for the onset of Alzheimer's with onset as early as 23 years of age. The PSEN2 mutation is the cause of less than 1% of autosomal dominant Alzheimer's cases, with environmental factors influencing these carriers more.
The review of different articles has led us to the conclusion that there is a relationship between PSEN and Alzheimer's. Currently, advances in genome sequencing techniques have provided a large amount of information about PSENs, their function, their location in our genes, their involvement in the formation of βA, etc. However, today there are still gaps in terms of the molecular mechanisms in which PSEN are involved.
Another major genetic risk factor is the presence of the APOE4 gene (apolipoprotein related to familial hyperlipoproteinemia and hypercholesterolemia), which tends to cause amyloid accumulation in the brain before it develops. the first symptoms of Alzheimer's appear. Thus, Aβ amyloid deposition tends to precede the symptoms of Alzheimer's.
Other evidence stems from the findings in genetically modified mice, which only express a mutated human gene, the APP gene, which invariably causes the development of fibrillar amyloid plaques. an experimental vaccine that caused the removal of these plaques but had no effect on dementia.
Plaque deposits have no correlation with neuronal loss.
This observation supports the tau hypothesis, which argues that it is this protein that initiates the cascade of Alzheimer's disease disorders. According to this model, hyperphosphorylated tau adopt anomalous forms, distributing themselves in long rows. They eventually form tangles of neurofibrils within the nerve cell bodies.
When this occurs, the microtubules disintegrate, collapsing the neuron's transport system. This can initiate the first dysfunctions in the biochemical communication between one neuron and the other and lead to the death of these cells.
According to a study carried out by a team of scientists from the University of Cambridge, in the United Kingdom, whose results are published in Brain, the tau protein, which causes the death of nerve cells, spreads throughout the brain in the Alzheimer's disease and thus blocking its spread can prevent the disease from breaking out.
Symptoms of Alzheimer's are thought to be caused by the buildup in the brain of two abnormal proteins: amyloid beta protein and tau protein. It is believed that amyloid beta is produced first, promoting the appearance and spread of tau, and that it is the latter that destroys nerve cells, impairing memory and cognitive functions.
Until a few years ago, it was only possible to observe the accumulation of these proteins by examining the brains of patients postmortem. However, recent developments in positron emission tomography (PET) have allowed scientists to begin to visualize its accumulation in patients who are alive.
The way in which tau is presented throughout the brain has been the subject of speculation among scientists, and three hypotheses have been proposed:
- One hypothesis is that the anomalous tau begins at a point and from there it spreads to other regions, triggering a chain reaction. This idea is known as "transneuronal production" and is supported by studies in mice. When a mouse is injected with an abnormal human tau protein, it spreads quickly throughout the brain. However, it should be recognized that the amount of tau injected is much higher than the tau levels observed in human brains and the protein spreads quickly by the brain of a mouse while slowly spreading through the human brain.
- The hypothesis of "metabolical vulnerability", which considers that tau protein occurs locally in nerve cells, but that some regions have greater metabolic demands and therefore are more vulnerable to protein. In these cases, tau is a marker of suffering in the cells.
- And the last hypothesis, of "trophic support", also suggests that some brain regions are more vulnerable than others, but that this has less to do with metabolic demand and more with the lack of nutrition in the region or with gene expression patterns.
Advances in PET scanning now allow comparisons between these hypotheses.
Scientists analyzed functional connections within the brains of Alzheimer's patients and compared them to tau levels. Their findings support the idea of transneuronal spread, that is, that tau starts in one place and spreads. At the same time, they found that the predictions for the last two hypotheses did not hold.
According to Thomas Cope, the first author of the study, transneuronal propagation is correct, the areas of the brain that are most connected have the highest accumulation of the abnormal tau protein and will transmit it to their connections. In Alzheimer's disease, the most common brain region for tau to appear first is the memory region, in the area of the entorhinal cortex, which is next to the hippocampus. The first symptoms in Alzheimer's tend to be memory problems, and Cope's study suggests that tau then spreads through the brain, infecting and destroying nerve cells as it goes, making the patient's symptoms progressively worse.
This confirmation is important because it indicates that the progression of Alzheimer's disease can be slowed or even stopped by developing drugs to prevent tau from moving through neurons.
Microbiological hypotheses
There are numerous hypotheses that have been put forward throughout history about the pathogenesis of Alzheimer's and that have not been confirmed by subsequent independent studies.
In 2013, a research team published a statistical study in which they found a correlation between disseminated fungal infections and Alzheimer's disease. This hypothesis has not been confirmed.
In 2018, a team hypothesized that the bacterium Porphyromonas gingivalis could be one of the causes of Alzheimer's disease. This hypothesis has not been confirmed either.
In 2020, a study correlated dysbiosis of the intestinal microbiota and the appearance of amyloid plaques in the brain, typical of Alzheimer's disease. This hypothesis has not been confirmed by subsequent studies.
Pathogenesis
Alzheimer's disease is characterized by loss of neurons and synapses in the cerebral cortex and in certain subcortical regions. This loss results in atrophy of the affected regions, including degeneration in the temporal and parietal lobes and parts of the frontal cortex and cingulate gyrus.
Neuropathology
Neurodegeneration in Alzheimer's disease is due to two processes: the first involves the beta-amyloid protein, which accumulates forming plaques on the outside of neurons. In turn, there is an alteration in the behavior of the tau protein, which begins to form interwoven fibers inside the nerve cell, the so-called tangles. Many individuals, in their old age, are likely to develop these plaques and tangles as part of the normal aging process. However, Alzheimer's patients have higher numbers in specific locations of the brain, such as the temporal lobe.
Biochemistry
Alzheimer's disease has been defined as a protein-unfolding disease, or proteopathy, due to the accumulation of abnormally folded Aβ and tau proteins in the brain.
Neuritic plaques are made up of small peptides 39-43 amino acids in length, called beta-amyloids (abbreviated A-beta or Aβ). Beta-amyloid is a fragment that comes from a larger protein known as Amyloid Precursor Protein (APP). This protein is essential for the growth of neurons, for their survival and post-damage repair.
In Alzheimer's disease, a still unknown process is responsible for the APP being split into several smaller fragments by enzymes that catalyze a proteolysis process.
One of these fragments is the beta-amyloid fiber, which clumps together and deposits outside neurons in microscopically dense formations known as senile plaques.
Alzheimer's disease is considered, due to the abnormal aggregation of the tau protein, as a tauopathy. Healthy neurons are composed of a cytoskeleton, an intracellular support structure, partially made of microtubules. These microtubules act as rails that guide nutrients and other molecules from the neuronal body to the ends of the axons and vice versa. Each tau protein stabilizes microtubules when it is phosphorylated and because of this association is called microtubule-associated protein. In Alzheimer's, tau, due to chemical changes that result in its hyperphosphorylation, binds with other tau strands creating tangles of neurofibrils and thus disintegrates the neuron's transport system.
Pathology
How the production and aggregation of Aβ (beta Amyloid) peptides play a role in Alzheimer's disease has not been fully explained.
The traditional formula of the amyloid hypothesis points to the accumulation of Aβ peptides as the main event leading to neuronal degeneration. The accumulation of amyloid fibers, which appears to be the abnormal form of the protein responsible for perturbing intracellular calcium ion homeostasis, induces programmed cell death, called apoptosis.
It is also known that Aβ accumulates selectively in the mitochondria of brain cells affected in Alzheimer's disease and that it is capable of inhibiting certain enzymatic functions, as well as altering the use of glucose by neurons.
Various inflammatory mechanisms and cytokine involvement may also play a role in the pathology of Alzheimer's disease. Inflammation is the general marker of tissue damage in any disease and may be secondary to the damage produced by Alzheimer's disease, or the expression of an immune response. Using DNA methylation data, it was estimated that granulocytes could be increased in patients with Alzheimer's. Similarly, it was determined that patients diagnosed with dementia had increased granulocytes, but to a lesser extent than other Alzheimer's patients, which could be a cause or consequence of disease progression.
But also, according to a new study, the decrease in estrogen production after menopause seems to make women more vulnerable to Alzheimer's.
Genetics
The vast majority of patients with this disease have or have had a relative with Alzheimer's. It must also be said that in a small proportion of patients, Alzheimer's is due to an autosomal dominant generation, which causes the disease to appear early. In less than 10% of cases, Alzheimer's appears before the age of 60 as a consequence of autosomal dominant mutations, representing barely 0.01% of all cases.
These mutations have been found in three different genes: the amyloid precursor protein (APP) gene, and the presenilin 1 and 2 genes. While the early-onset form of Alzheimer's disease occurs by mutations in three basic genes, the most common form has not been explained with a purely genetic model. The presence of the apolipoprotein E gene is the most important genetic risk factor for Alzheimer's disease, but it cannot explain all cases of the disease.
In 1987, the association of Alzheimer's disease with chromosome 21 was discovered. This was important because most people with Down syndrome, or trisomy of chromosome 21, have neuropathological lesions similar to those of Down syndrome. alzheimer. Within chromosome 21 we find the PPA gene. John Hardy and his collaborators in 1991 stated that this gene was involved in Alzheimer's disease in a small number of families. However, it is considered that between 5-10% of relatives with early disease suffer from it due to a mutation of this gene.
Research within this gene has focused on the Ab peptide (all mutations are around this peptide).
The mutations produced increased concentrations of the Ab peptide. This led to the formation of the "amyeloid cascade" hypothesis in the 1990s.
The «amyeloid cascade» consists of the fact that the great production of Ab would lead to the formation of deposits in the form of senile plaques. These senile plaques would be harmful to cells leading to neurofibrillary tangles, cell death and dementia.
Later, the linkage of Alzheimer's disease with chromosome 14 was seen in a large group of families. But this led to a chain of errors and with it erroneous conclusions.
Rudy Tanzi and Peter St George-Hyslop in 1995, using cloning techniques, discovered another gene S182 or Presenilin-1 (PS1). This gene is found between transmembrane domains 9 and 8 (with two hydrophilic regions) and more than 30 mutations have been found.
This gene is involved in apoptosis processes and is essential during development.
Most mutations of the Presenilin-1 (PS1) gene cause a change in the primary structure. PS1 and Alzheimer's disease do not have a clear relationship, but it is noteworthy that the patients had mutations that increase Ab in plasma.
Shortly later, a new gene called presenilin-2 (PS2) was discovered and it also causes an increase in Ab concentration, although the observed mutations are smaller than the other genes (PPA and PS1). PS2 is made up of 8-9 transmembrane domains.
Most of the mutations in the APP gene and in those of the presenilins, increase the production of a small protein called beta-amyloid (Abeta 2), which is the main component of senile plaques.
Although most cases of Alzheimer's do not run in families, certain genes act as risk factors. An example is the familial transmission of the e4 allele of the apolipoprotein E gene. This gene is considered a risk factor for the appearance of sporadic Alzheimer's in late stages, causing 50% of Alzheimer's cases. In addition to this, around than 400 genes have also been investigated for their association with late-stage sporadic Alzheimer's. For example, in a GWAS meta-analysis published in 2019 the authors identified 16 genes significantly associated with late-onset Alzheimer's and noted that 7 of they (HLA-DRA, HLA-DRB1, PTK2B, CLU, MS4A3, SCIMP and RABEP1) were not located in the APOE locus, so they could also be of great interest for future lines of research in this neurodegenerative disease. In a new genome-wide association study (GWAS) published in 2021, identified 7 new genes (TNIP1, HAVCR2, TMEM106B, GRN, LILRA5, AGRN, NTN5) associated with the development of sporadic or late-onset Alzheimer's (LOAD) not localized to the APOE locus. 5 of these 7 genes (TNIP1, HAVCR2, LILRA5, AGRN, TNT5) had not previously been associated with the development of neurodegenerative diseases. These new possible causal variants of the disease are of great interest since they could be used as new therapeutic targets for the treatment of Alzheimer's.
Epigenetics
In addition to these genetic variants identified by GWAS, epigenetic modifications have also been shown to play an important role. In a joint methylome-wide association study (MWAS), which also included Parkinson's and ALS cohorts, it was determined that there were 12 differentially methylated positions in patients with these neurodegenerative diseases. The strongest association occurred in the promoter region of the FKBP5 gene. The expression of this gene increases progressively with age and this increase would correlate with an increase in tau pathology.
Thus, geneticists agree that there are more genes that act as risk factors, although they also affirm that there are others that have certain protective effects that lead to delaying the age of onset of Alzheimer's. An example is the alteration in the reelin gene, which contributes to increasing the risk of Alzheimer's disease in women.
Clinical picture
Predementency
The first symptoms are often confused with old age or stress in the patient. A detailed neuropsychological evaluation is capable of revealing mild cognitive difficulties up to 8 years before the person meets the diagnostic criteria.
These early signs can have an effect on activities of daily living.
The most notable impairment is memory loss, manifested as difficulty remembering recently learned facts and an inability to acquire new information.
Mild difficulties in executive functions —attention, planning, flexibility, and abstract reasoning— or disorders in semantic memory —remembering the meaning of things and the interrelationship between concepts— may also be symptoms in the early stages of Alzheimer's.
Apathy may appear, being one of the persistent neuropsychiatric symptoms throughout the disease.
The preclinical phase of the disease is called by some mild cognitive impairment, but there is still debate about whether the term corresponds to an independent diagnostic entity or if, indeed, it is the first stage of the disease. disease.
Initial dementia
Symptoms in this early phase range from a simple and insignificant, but sometimes recurring, memory loss (such as difficulty orienting oneself in places such as streets while driving the car), to a constant and more persuasive loss of memory. of memory known as short-term memory, presenting difficulties when interacting in areas of a familiar nature such as the neighborhood where the individual lives.
In addition to recurrent memory loss, a small portion of patients present difficulties with language, recognition of perceptions —agnosia— or execution of movements —apraxia— with greater prominence than memory disorders.
Alzheimer's doesn't affect memory abilities in the same way. Long-term or episodic memories, as well as semantic or factual memory and implicit memory, which is body memory about how to perform actions (such as holding a fork to eat).), are affected to a lesser degree than the abilities to learn new facts or create new memories.
Language problems are mainly characterized by reduced vocabulary and decreased fluency of words, which leads to a general impoverishment of spoken and written language. The Alzheimer's patient is usually able to adequately communicate basic ideas.
There is also clumsiness when performing fine motor tasks, such as writing, drawing or dressing, as well as some coordination and planning difficulties.
The patient maintains his autonomy and only needs supervision when it comes to complex tasks.
At this stage it is common for the person to get disoriented on the street and get lost, so it is recommended to take precautions:
- Putting on the wrist a bracelet with a contact phone number.
- Notifying those who know the situation, to alert the family in case of finding the alzhéimer patient wandering.
- Using a GPS locator for people with alzhéimer, with which the family can always know where it is. There are tele-assistance locators, in which the caregiver should call a teleoperator to know the location of the patient who carries the device, and direct locators, in which the caregiver has a receiver with which, pressing a button, sees on the screen a map and the exact position of the sick person.
Moderate dementia
As the disease progresses, patients can perform tasks with some independence (such as using the bathroom), but will require assistance for more complex tasks (for example, going to the bank, paying bills, etc.). Gradually, the Loss of skills, such as recognizing objects and people. In addition, behavioral changes such as violent outbursts can occur even in people who have never exhibited this type of behavior.
Language problems are increasingly evident due to an inability to remember vocabulary, which leads to frequent mistaken word substitutions, a condition called paraphasia. Reading and writing abilities progressively worsen.
Complex motor sequences become less coordinated, reducing the person's ability to perform routine activities.
During this phase, memory disorders also worsen and the patient begins to stop recognizing their family members and closest ones.
Long-term memory, which until then remained intact, deteriorates.
At this stage, changes in behavior become more noticeable. The most common neuropsychiatric manifestations are distractions, drifting, and confusional episodes at the end of the day (aggravated by fatigue, low light, or darkness), as well as irritability and emotional lability, including inappropriate crying or laughing., unpremeditated aggression and even resistance to the people in charge of their care. In approximately 30% of patients illusions appear in the recognition of people. Urinary incontinence can also appear.
These symptoms stress family members and caregivers and may be reduced by transfer to a long-term care facility.
Advanced dementia
The disease brings deterioration of muscle mass, loss of mobility, which leads the patient to a state of bedridden, the inability to feed himself, along with incontinence, in those cases in which death is not has still arrived due to external causes (infections due to ulcers or pneumonia, for example).
Language becomes severely disorganized, leading to complete loss. Despite this, the ability to receive and send emotional signals is preserved.
Patients will not be able to perform even the simplest tasks by themselves and will require constant supervision, thus remaining completely dependent. Some aggressiveness may still be present, although it is more common to see extreme apathy and exhaustion.
Symptoms and stages
The main symptoms of Alzheimer's are short-term memory loss, anosognosia (ignorance of the disease), confabulations to cover the gaps in short-term memory (they lie or invent things to fill the gap or gap in their stories), depressive state, attention problems, problems with orientation, personality changes, difficulties with language and inexplicable mood swings, disorientation, among others. This disease has three stages in which it presents different symptoms.
Stage 1 or mild
When the disease begins to manifest itself, people with Alzheimer's tend to be less energetic and spontaneous. They show minimal memory loss and mood swings, and are slow to learn and react. They also become isolated, avoiding unfamiliar people and new places and preferring the familiar. Individuals become confused, have difficulty organizing and planning, are easily lost, and exercise poor judgment. They may have difficulty performing routine tasks, and have difficulty communicating and understanding written material. If the person is employed, memory loss may begin to affect job performance. All this causes them frustration and anger.
Stage 2 or moderate
At this stage, the person with Alzheimer's disease can still perform simple tasks independently, but may need help with complicated activities. Patients forget recent events and their personal history, and are increasingly disoriented and disconnected from reality. They may confuse their past with the present, and have a hard time understanding the current situation, date and time. They may also have trouble recognizing familiar people. Problems with speaking and comprehension increase, reading and writing are more difficult, and the individual tends to make up words. Those affected can no longer be safe alone and can wander. As Alzheimer's disease patients become more aware of this loss of control, they may become depressed, irritable and restless, or apathetic and withdrawn. They may experience sleep disturbances and have difficulty eating, dressing and grooming.
Stage 3 or severe
During this final phase, people may lose the ability to feed themselves, speak, recognize people, and control of bodily functions. His forgetfulness worsens and can become almost complete. Constant attention is necessary. In a weakened physical state, the patient may become vulnerable to other diseases and respiratory problems, especially when confined to bed.
Diagnosis
The diagnosis is based first on the history and clinical observation, by the health professional and that which is referred by the relatives, based on the neurological and psychological characteristics, as well as on the absence of alternative conditions: a diagnosis of exclusion.
Then for a few weeks or months, memory and functioning tests or intellectual evaluation are done. Blood tests and scans are also done to rule out alternative diagnoses.
There is no pre-mortem test to conclusively diagnose Alzheimer's. It has been possible to approximate the certainty of the diagnosis to 85%, but the definitive one must be made with histological tests on brain tissue, generally obtained at autopsy.
Brain imaging tests—computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), or single photon emission computed tomography—can show different signs of dementia, but they do not specify what dementia it is.
Therefore, the diagnosis of Alzheimer's disease is based both on the presence of certain neurological and neuropsychological characteristics, as well as on the absence of an alternative diagnosis, and relies on brain scanning to detect signs of dementia. New diagnostic techniques based on electroencephalographic signal processing are currently being developed.
Once identified, the average life expectancy of patients living with Alzheimer's disease is approximately 7 to 10 years, although there are known cases in which the terminal stage is reached earlier, between 4 and 5 years; there is also the other extreme, where they can survive up to 21 years.
Diagnostic criteria
The Alzheimer's Association is the body that has established the most commonly used diagnostic criteria, listed in the NINCDS-ADRDA Criteria for Alzheimer's.
These guidelines require that the presence of a cognitive disorder and the suspicion of a dementia syndrome be confirmed with a neuropsychological evaluation with a view to categorizing the diagnosis of Alzheimer's into two: possible or probable. Histologic confirmation, which includes microscopic examination of brain tissue, is required for a definitive diagnosis of Alzheimer's. These criteria include that the presence of a cognitive disorder and the suspicion of a dementing syndrome be confirmed by neuropsychological evaluations to distinguish between a possible and a probable diagnosis of Alzheimer's disease. Reliability and statistical validity have been shown between the diagnostic criteria and the definitive histological confirmation.
Eight cognitive domains are most frequently damaged in Alzheimer's: memory, language, perception, attention, constructive and orientation skills, problem solving, and functional abilities. These parameters are equivalent to those evaluated in the NINCDS-ADRDA Criteria published by the American Psychiatric Association.
Diagnostic tools
Neuropsychological assessments, including the minimental exam, are widely used to assess for cognitive disorders necessary for the diagnosis of AD. Another series of more comprehensive examinations are necessary for greater reliability in the results, especially in the initial phases of the disease.
Neurologic examination in early Alzheimer's is crucial for the differential diagnosis of Alzheimer's and other diseases.
Interviews with relatives are also used to assess the disease. Caregivers can provide important information and details about routine skills as well as the decline over time in the patient's mental function.
The point of view of the person in charge of the patient is especially important because the patient is usually unaware of his own shortcomings.
Often, family members have challenges detecting the early symptoms and signs of dementia and may not accurately communicate the information to the specialized health professional.
Additional tests can provide information about some elements of the disease and tend to be used to rule out other diagnoses. Blood tests can identify causes of dementia other than Alzheimer's, which may, in rare cases, be reversible diseases.
Psychological testing for depression would be valuable, as depression can co-occur with Alzheimer's, or be the cause of cognitive disorders.
Where specialized neurological imaging, such as PET or single photon tomography, is available, it can be used to confirm the diagnosis of Alzheimer's along with assessments of the individual's mental status.
The ability of a single photon emission computed tomography scan to distinguish between Alzheimer's and other possible causes in someone who has already been diagnosed with dementia appears to be superior to diagnostic attempts through mental examinations and patient history.
A new technique, known as PiB PET, has been developed to directly and clearly image beta-amyloid deposits in vivo, using a radiopharmaceutical that binds selectively to Aβ deposits.
Another recently marked target of Alzheimer's disease is analysis of cerebrospinal fluid for beta amyloid or tau proteins.
Both advances in medical imaging have led to proposals to change the diagnostic criteria.
Markers for diagnosis
One of the main objectives of the diagnosis would consist of the identification of genetic markers that would allow a diagnosis of Alzheimer's in the initial stages or even before the development of the disease itself. Genome association studies (also called GWAS) are useful for determining these biomarkers. A study published in 2019 has observed through inversion genotyping and genome association analysis (GWAS) an inversion that could be related to the risk of Alzheimer's, because it presents linkage disequilibrium with a SNP associated with Alzheimer's.
Treatment
Alzheimer's disease is currently incurable and terminal.
The treatment of Alzheimer's is based on two complementary pillars: non-pharmacological treatment and pharmacological treatment. Psychosocial interventions are used in conjunction with drug treatment.
Pharmacological treatments
Anticholinesterase drugs have been proven to be somewhat effective, they have an inhibitory action on cholinesterase, the enzyme responsible for breaking down acetylcholine (a neurotransmitter that is missing in Alzheimer's disease and that substantially affects memory and other functions cognitive). New drugs that intervene in the regulation of glutaminergic neurotransmission have been incorporated into the treatment of the disease. With all this, the behavior of the patient has improved a little in terms of apathy, initiative, functional capacity and hallucinations, improving their quality of life. However, it should be noted that since 2008 the records of the improvement obtained with these drugs are discreet, that is, they have not been able to alter the course of the underlying dementia.
The first commercialized anticholinesterase drug was tacrine, which is no longer used today due to its hepatotoxicity. In 2008, in Europe and North America there were 4 drugs available, three of them are acetylcholinesterase inhibitors: donepezil (marketed as Aricept), rivastigmine (marketed as Exelon or Prometax) including the Exelon patch, and Galantamine (marketed as Reminyl).
All three have a similar efficacy profile with similar side effects. The latter are usually gastrointestinal disorders, anorexia and heart rhythm disorders. The fourth drug is an NMDA receptor antagonist, memantine. None of the four is indicated to slow or stop the progress of the disease.
Reduced activity of cholinergic neurons is one of the recognized hallmarks of Alzheimer's disease.
Acetylcholinesterase inhibitors are used to reduce the rate of acetylcholine degradation, thus maintaining adequate concentrations of the neurotransmitter in the brain and stopping its loss caused by the death of cholinergic neurons.
There is some evidence that these drugs are effective in mild and moderate stages of the disease, though somewhat less useful in the advanced phase. Only donepezil has been approved for this state of dementia.
The use of these drugs in mild cognitive disorders has not been shown to be able to delay the onset of Alzheimer's.
The most common adverse effects include nausea and vomiting, both linked to the cholinergic excess that results from them. These effects appear between approximately 10 and 20% of those treated and are mild to moderate in severity. Less frequent side effects include muscle cramps, decreased heart rate, decreased appetite and body weight, and increased production of gastric juice.
Memantine is a drug with a different mechanism of action, which is indicated in the moderate and advanced phases of the disease. Its theoretical mechanism of action is based on antagonizing glutaminergic NMDA receptors, originally used as an anti-influenza agent. Glutamate is an excitatory neurotransmitter of the central nervous system. Apparently, an excess of glutaminergic stimulation could produce or induce a series of toxic intraneuronal reactions, causing cell death by a process called excitotoxicity, which consists of an overstimulation of glutamate receptors. This excitotoxicity occurs not only in Alzheimer's patients, but also in other neurodegenerative diseases, such as Parkinson's disease and multiple sclerosis.
Clinical trials have shown moderate efficacy in these patients and an acceptable side effect profile. In 2005, its indication in moderate phases of the disease was also approved, but the effects in the initial phases are still unknown.
Adverse effects of memantine are rare and mild and include hallucinations, confusion, dizziness, headache, and fatigue.
The combination of memantine and donepezil has been shown to be statistically significant but marginally successful from a clinical point of view.
There are also drugs that improve some of the symptoms produced by this disease, among which are anxiolytics, hypnotics, neuroleptics and antidepressants. Antipsychotic drugs are indicated to reduce aggression and psychosis in Alzheimer's patients with conduct problems, but they are used sparingly and not routinely because of serious side effects such as cerebrovascular events, extrapyramidal disorders, and cognitive decline..
Non-pharmacological treatments
Slowing the progression of Alzheimer's
The progression of the disease can be faster or slower depending on the environment of the person with Alzheimer's. It is not an easy situation and the family will have to make great efforts to offer the person with Alzheimer's the most favorable environment possible.
Disease accelerators. The following situations are considered accelerators: family stress, sudden changes in daily routines, moving to a new and unknown address (such as nursing homes).
Disease retardants. The following situations are considered retardants: happy family environment, exercising, socializing with friends or other people.
Psychosocial intervention
There is some evidence that stimulating cognitive abilities helps slow down the loss of these functions and abilities. This stimulation consists of working on those areas that the patient still has, so that the training makes it possible to compensate for the losses that the patient is suffering with the disease.
Psychosocial interventions are used in conjunction with pharmacological treatment and are categorized into behavioral, emotional, cognitive, and arousal-oriented approaches. Research on the effectiveness of these interventions is not yet available and, in fact, is rarely specific to Alzheimer's, focusing on dementia in general.
Behavioral interventions attempt to identify and reduce the antecedents and consequences of behavior problems. This approach has not been shown to be successful in improving the patient's general functioning, especially in relation to her environment, but it has been able to help reduce certain specific behavioral problems, such as urinary incontinence.
There is still a lack of quality data on the effectiveness of these techniques in other problems such as patient wandering.
Emotionally oriented interventions include validation therapy, reminiscence therapy, supportive psychotherapy, sensory integration (also called snoezelen), and stimulating presence therapy. Supportive psychotherapy has had little formal scientific study, but some specialists find it useful in patients with mild disorders. Reminiscence therapy involves discussion of past experiences individually or in a group, often with the aid of photographs., household objects, music and recordings or other belongings from the past. In this therapy, likewise, there are not many quality studies on its effectiveness, although it can be beneficial for cognitive restructuring and mood.
The treatment with stimulated presences is based on the adherence theories and involves listening to recorded voices of the relatives and closest loved ones of the patient with Alzheimer's. Preliminary evidence indicates that such activities reduce anxiety and challenging behaviors.
Finally, validation therapy is based on the acceptance of reality and the personal experience of other people, while sensory integration is based on guided exercises that stimulate the senses. There is not yet enough evidence to support the use of these therapies in patients with Alzheimer's.
The goal of cognitive behavioral therapies, including counseling and cognitive rehabilitation, is to reduce cognitive distortions. Reality orientation consists of presenting information about the time, place, or person in order to ease their understanding of their surroundings and their place in those places. On the other hand, cognitive training attempts to improve weakened abilities by exercising the mental abilities of the patient. Both exercises have shown some effectiveness in improving cognitive abilities.
However, in some studies these effects were transient and in others they had a negative effect, adding to the patient's frustration, according to reports.
Stimulation-oriented treatments include art therapy, music therapy, and pet-assisted therapies, physical exercise, and any recreational activity. Stimulation has modest support when applied with the intention of improving the patient's behavior, mood, and, to a lesser degree, functioning. Although they are important effects, the main benefit reported among stimulation therapies is the improvement in the patient's daily life routines.
Care
Because there is no cure for Alzheimer's, over time the patient falls into a state of inability to self-sufficiently care for himself, so third-party care is a vital measure for that deficiency and must be carefully approached during the course of the disease.
In the early and moderate phases, modifications to the patient's living environment and lifestyle can provide security and reduce burdens on the caregiver.
A few examples of such modifications are adherence to simplified routines, such as the placement of padlocks, the use of a wristband with the caregiver's phone number (or more advanced solutions such as a GPS locator), the labeling of household objects and the use of modified utensils for daily living. It may reach the point where the patient is not able to feed himself, so he must start eating his food in smaller portions or on diets not solid with the help of other people. When swallowing difficulties appear, the use of gastric tubes may be indicated. In such cases, the medical and ethical effectiveness of having to continue feeding the patient are important considerations for caregivers and family members of the individual.
Physical restraints are rarely indicated at any stage of the disease, although there are situations in which they are necessary to prevent the Alzheimer's patient from harming himself or others.
As the disease progresses, different medical manifestations may appear, such as oral and dental diseases, pressure ulcers, malnutrition, hygiene problems or respiratory, urinary, skin or eye infections, among others. Careful patient management can prevent such problems, but if they do occur, they should be treated under medical supervision. During the final stages of the disease, treatment focuses on maintaining quality of life until death.
Treatments under investigation
Vaccines
Vaccine experiments are also underway, based on the idea that if the immune system can be trained to recognize and attack beta-amyloid plaque, it could reverse amyloid deposition and stop disease. Initial results in animals were promising. However, when the first vaccines were tested in humans in 2002, brain inflammation (meningoencephalitis) occurred in a small proportion of study participants, so testing was stopped. The participants were continued to be studied and an improvement in the slowness of the disease progress was observed. It has recently been discovered that brain inflammation was produced by a series of peptides that were included in the AN-179 vaccine, so the creation of a vaccine that does not have these peptides in its composition is being investigated.
A vaccine, ABvac40, is being tested as a preventive against Alzheimer's since 2014. Its objective is to stop the production of amyloid plaques. The vaccine would produce antibodies responsible for eliminating amyloid beta 40 and 42, which are the cause of brain neurodegeneration. Vaccine trials will be conducted on a total of 24 people: 16 diagnosed and mild-stage patients and eight patients receiving placebo. If its safety is proven, the vaccine will not be on the market before 2018.
Ultrasound
In March 2015, a completely new approach to Alzheimer's was published in Science-Translational Medicine, which has been tested in mice.
It uses a particular way of applying ultrasound, inside the gray brain tissue. These sound waves turned out to be able to gently open the blood-brain barrier, which separates the brain from the blood, and stimulated del Río Hortega cells, or microglia. These microglial cells, once activated, were able to gradually disintegrate and eliminate the beta-amyloid clumps of Alzheimer's. The research authors reported seeing complete restoration of memories in 75% of the mice they tested. They found that the mice thus treated displayed memory improvements in three specific tests. The scientific team plans to start testing with higher laboratory animals, such as sheep and apes, and hopes to be cleared to start human trials in 2017.
For its part, in classical clinical (pharmacological) approaches, a 2014 study stated that in mice the antidepressant citalopram stopped the growth of existing Alzheimer's disease beta-amyloid plaques and reduced the formation of new plaques by a 78% In a second experiment, the scientists administered a single dose of citalopram to 23 people between the ages of 18 and 50 who were neither cognitively impaired nor suffering from depression. When they obtained cerebrospinal fluid samples at 24 hours, they observed a 37% reduction in the production of the beta-amyloid protein.
If this disease is related to insulin resistance, multiple therapeutic alternatives are presented. The use of drugs used in the treatment of diabetes is currently being evaluated. Recent studies show that intranasal administration of insulin improves cognitive function in normal and Alzheimer's patients.[citation needed] A systematic review of the clinical trials carried out so far shows encouraging results. On the other hand, the use of enzyme induction techniques has been proposed, with enzymes activated by insulin.[citation needed]
Stem cells
Another area of research is regenerative medicine. It involves injecting embryonic or adult stem cells into the patient's brain to try to stop cognitive decline. Human experiments have already been carried out with positive results.[citation needed]
Brain pacemaker
Brain stimulation attempts to normalize activity, with a device called a neurostimulator, similar to a cardiac pacemaker. The device is part of a treatment called deep brain stimulation (DBS), which involves the release of electrical impulses to regulate brain activity. The research, carried out at the Johns Hopkins School of Medicine, is part of a larger project initiated in Canada, where pacemakers have already been implanted in six patients with the disease. The treatment made the patients - all with moderate forms of Alzheimer's - show an increase in neural activity for 13 months.
Deep brain stimulation therapy has been used with people with Parkinson's disease. Now, the therapy could be an alternative to reverse the cognitive deterioration of people with Alzheimer's.
This functional neurosurgery seeks to repair, modulate or correct a deficit in a specific neurological system or network. What happens with Alzheimer's is that brain chemistry is altered and this leads to abnormal electrical activity that can be expressed in tremors, cognitive impairment or psychiatric disorders. The Alzheimer's app is still in its early stages.
Prevention
Global studies on the different measures that can be taken to prevent or delay the onset of Alzheimer's disease have had conflicting results and a causal relationship between risk factors and the disease has not yet been proven, nor have they been confirmed. attributed to specific side effects. At the moment, there do not appear to be definitive measures to prevent the onset of Alzheimer's.
Several epidemiological studies have proposed various relationships between certain modifiable factors, such as diet, cardiovascular risks, pharmaceuticals or intellectual activities, among others, and the probability that Alzheimer's disease will appear in a population. For now, more research and clinical trials are needed to see if these factors help prevent it.
The Mediterranean diet has been associated with a lower risk of developing Alzheimer's disease, due to its role in preventing the development of cardiovascular disease and its anti-inflammatory and antioxidant effects.
Curcumin in curry has shown some efficacy in preventing brain damage in mouse models in studies from 2001 and 2007.
Similar properties were reported in 2010 and 2012 for tests in mice of Withania somnifera (ashwagandha, Indian ginseng).
Although cardiovascular risks, such as high cholesterol, high blood pressure, diabetes, and smoking, are associated with an increased risk of Alzheimer's disease development and progression, statins, which are drugs that lower the concentration of cholesterol in blood plasma, have not been effective in preventing or ameliorating Alzheimer's. However, in some individuals, long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) is associated with a reduced likelihood of developing it.
Other drugs and therapies, such as hormone replacement in women, are no longer recommended as preventive measures for Alzheimer's.
A 2007 report is also included that concluded the lack of significant evidence and the presence of inconsistencies in the use of ginkgo biloba to improve cognitive disorders.
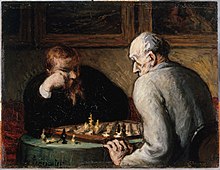
Different intellectual activities, such as playing chess, Go, reading, doing crossword puzzles, or frequent social interactions, appear to slow the onset and reduce the severity of Alzheimer's. Speaking multiple languages also appears to be linked to the late onset of the disease.
Other studies have suggested a possible increased risk of Alzheimer's disease with exposure to magnetic fields, ingestion of metals, particularly aluminum, or exposure to certain solvents. The quality of some of these studies have been criticized, and other studies have concluded that there is no relationship between these environmental factors and the onset of Alzheimer's.
Some scientific associations currently work in the medical and social field, recommending and/or advising the families of patients, in turn promoting research, such as the Alzheimer's Association and Alzheimer Argentina.
Contenido relacionado
Ductal carcinoma
Drill Index
Suicide